Osteoporosis (bone loss) is one of the most important common diseases. In Germany, millions of people suffer from it, especially older women. In those affected, the bone substance builds increasingly degraded. This makes the bones increasingly unstable and brittle. Read here everything important about causes, symptoms, therapy and prevention of osteoporosis!
Quick Overview
- What is osteoporosis? Metabolic disease of the bones, in which more and more bone tissue is broken down (bone loss). The bones can break more easily.
- symptoms: at the beginning often no complaints. In the course of ongoing pain such as back pain, broken bones in trivialities or no apparent cause (spontaneous fractures), increasing hunchback (“widow’s hump”) and decreasing body size.
- Causes: Primary osteoporosis occurs in older age and after menopause (estrogen deficiency!). Secondary osteoporosis is the result of other diseases or medications (hyperthyroidism, cortisone, etc.).
- Treatment: non-medical measures such as adequate exercise (exercise, physiotherapy) and proper nutrition; Calcium and vitamin D supplements; Osteoporosis drugs (bisphosphonates etc.); Treatment of underlying diseases (in secondary osteoporosis); possibly surgery for bone fractures
- Forecast: Osteoporosis is not curable so far. All the more important is an early diagnosis and treatment. Otherwise, the bone loss progresses on and on. This then means increasing pain and frequent fractures.
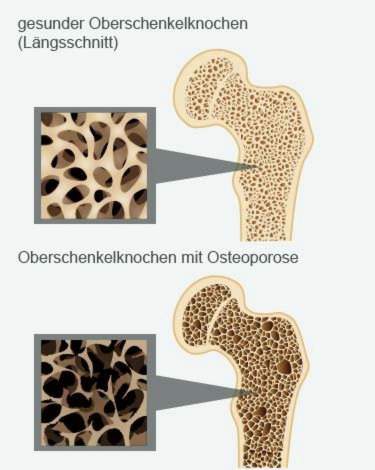
What happens with osteoporosis?
Bones consist of two basic building blocks:
- a special fabric that gives them shape and stability (Matrix)
- various minerals that are incorporated into the matrix (especially calcium and phosphate). They consolidate and strengthen the structure.
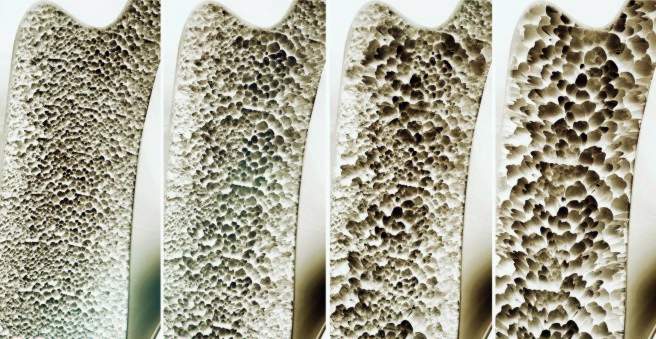
The bones are constantly being rebuilt to meet changing needs. By about the age of 35, more bone mass is generally built up than mined. From the age of 35, the bone is gradually outgrown and accelerates with age. Healthy older people lose about 0.5 to 1 percent of their bone mass every year.
This normal bone metabolism can be disturbed by a variety of influences. For example, calcium deficiency, lack of exercise and hormone-related diseases can cause the Bone structure inhibited and / or bone resorption promoted becomes. As a result, the bone mass disappears – it arises osteoporosis, Most affected are older people. In extreme cases, patients can lose up to six percent of their bone mass per year!
Osteoporosis: who is affected?
Osteoporosis usually occurs in old age. In Germany, about one quarter of all people over the age of 50 have osteoporosis. That’s about 7.8 million people.
This shows a difference between the sexes: about every third woman after the menopause and every fifth older man suffer from bone loss.
Almost all patients (95 percent) have a so-called primary osteoporosisIt is caused either by the estrogen deficiency after menopause (in women) or by the increased bone loss in older age (both sexes).
Only in a few osteoporosis patients (5 percent) is bone loss due to other diseases or drugs (secondary osteoporosis). Here more than half of those affected are men.
Special form: transient osteoporosis
A special form of the disease is the so-called transient osteoporosis. It mainly affects men of middle age. But women in the last trimester of pregnancy are affected more often.
Transient osteoporosis is one rapidly progressive, painful bone loss near the joint, Mostly the hip joint is affected. The patients have severe pain in the joint. This is also limited in his mobility.
Transient osteoporosis can be clearly diagnosed using magnetic resonance imaging (MRI). In the vicinity of the joint an extensive swelling (edema) in the bone marrow can be detected. The transient osteoporosis is in response to this local bone marrow edema considered. Therefore, it is also called bone marrow edema syndrome.
What exactly triggers the development of transient osteoporosis is not known. Circulatory disorders in the bones, overloading of the hip joints and traumas (such as a fall on the hip) are discussed.
The most important therapy measure is the affected one Relieve joint completely, In most cases, the disease heals spontaneously within several months (unless complications such as bone fracture occur). The pain can be with you drugs (like ibuprofen).
According to current knowledge, transient osteoporosis does not lead to permanent (chronic) complaints.
Osteoporosis: symptoms
Osteoporosis usually develops slowly. Initially, therefore, sufferers generally have no complaints. Only in the further course occur Pain on, for example, back pain and knee pain. They are often not recognized as the first symptoms of osteoporosis.
Some patients are also affected bone fractures: Often they are the result of trivial injuries. So even a small, harmless fall can cause a forearm break. Even spontaneous fractures without apparent cause are possible first symptoms of osteoporosis.
In the advanced stage of osteoporosis occur Increases fractures without cause on. Typical osteoporosis symptoms often include fractures close to the hip (such as fractures of the femoral neck), fractures of the upper and lower arms and vertebral bodies (vertebral body fracture).
Vertebral fractures
Sometimes in osteoporosis vertebral bodies slowly collapse. The affected people often do not notice it. These “creeping fractures “ cause no pain. They are therefore often not recognized and remain untreated. However, they cause the Body size decreases, With several vertebral fractures, it can even shrink by several centimeters! In addition, a can hunchback train (“widow’s hump”).
Also acute vertebral body fractures are possible signs of osteoporosis. In contrast to creeping fractures, pains appear very well, and indeed distinctly. In addition, the mobility is considerably limited in everyday life.
In general, the following symptoms may indicate vertebral fractures:
- severe, local, stabbing to burning back pain
- persistent back pain
- Decrease in height
- Curvature of the spine
Femoral neck fracture
Thigh cervicals are among the most serious complications of osteoporosis. Symptoms such as severe pain in the hip joint and a malposition of the affected leg indicate such a femoral neck fracture. In addition, the affected hip joint can no longer be charged.
vicious circle
Each fracture increases the risk of further fractures. For fear of recurrent fractures, osteoporosis patients often become insecure and anxious while walking and often fall off. This increases the risk of falling.
In addition, muscle strength diminishes in old age. In addition, many older people can hear and see worse. This affects the balance, which additionally aggravates the risk of falling. This increases the risk of fractures even further. Those affected fall into a vicious circle of fear and insecurity, increased risk of falling and new fractures, which further ignite the fear.
Osteoporosis: causes and risk factors
In principle, two groups of osteoporosis are distinguished: primary osteoporosis and much less common secondary osteoporosis.
Primary osteoporosis: causes
Primary osteoporosis occurs in postmenopausal women and in both sexes at older ages:
Of the Bone loss after menopause (postmenopausal osteoporosis) is hormonal: The female sex hormones (estrogens) regulate the formation and action of calcitonin and vitamin D. These two hormones are important for bone formation. During menopause, estrogen production declines. That is why many women develop bone loss after the last menstrual period.
Sex hormones (such as testosterone) are also important for bone metabolism in men. With them, however, the testosterone production is not stopped in middle age. Therefore, osteoporosis is less common in men than in women.
in the higher age Every person increasingly loses bone mass. This can cause osteoporosis in both men and women. Doctors speak of this senile osteoporosis.
Overall, different favor risk factors the development of osteoporosis. Nutrition that is little bone friendly (such as low-calcium diet), as well lack of exercise are the first to be mentioned here.
Especially from the age of 70 introduces dietary deficiency of calcium and vitamin D. to bone loss. Excessive diets, over-consumption of coffee, abuse of laxatives, and too much dietary phosphate cause the bones to get too little calcium and vitamin D. This favors osteoporosis.
Also excessive consumption of alcohol and nicotine are considered risk factors for bone loss.
In addition, osteoporosis frequently occurs in certain families. Experts therefore suspect that too genetic factors play a role.
Secondary osteoporosis: causes
Unlike primary osteoporosis, secondary osteoporosis is the result of other diseases or their treatment (medication).
For example, a secondary osteoporosis can be caused by a too much cortisone caused in the body. Such cortisone surplus is caused either by diseases like that Cushing’s syndrome or by one Long-term therapy with cortisone.
Also one Hyperthyroidism (hyperthyroidism) can cause osteoporosis: The excess of thyroid hormones accelerates the metabolism and promotes bone loss. At a Hyperfunction of the parathyroid gland Osteoporosis also often occurs. This is because too much parathyroid hormone is released. This hormone is an antagonist of calcitonin and vitamin D: it dissolves calcium out of the bones and thus promotes their degradation.
Other secondary causes of osteoporosis include:
- hormone-related diseases such as hypofunction of the gonads (ovaries, testicles), adrenal over-function, type 1 diabetes
- Stomach and intestinal diseases such as Crohn’s disease, ulcerative colitis, lactose intolerance, lactose intolerance, celiac disease: The use of important nutrients such as calcium is disturbed.
- malignant tumors (like bone metastases)
- severe chronic renal failure (renal insufficiency): Here, the body excretes a lot of calcium. So that the calcium level in the blood does not sink too much, calcium is released from the bones and absorbed into the blood.
- Inflammatory rheumatic diseases like rheumatoid arthritis (“rheumatism”)
- Other diseases like anorexia or cirrhosis (malnutrition favors osteoporosis)
- medications: In addition to cortisone, other medicines can promote osteoporosis, such as anticonvulsants, cyclosporin (after organ transplants, skin diseases, etc.), heparin (long-term thrombosis prevention therapy), and certain hormonal therapies (such as prostate cancer).
Osteoporosis: examinations and diagnosis
If you have the slightest suspicion of osteoporosis such as bone fracture without apparent cause (spontaneous fracture), you should go to the doctor. The earlier the bone loss is treated, the sooner the progression of the disease can be stopped. In addition, all people with an increased bone fracture risk will have an osteoporoticbasic diagnosis recommended. It consists of several parts:
Doctor-patient conversation
First, the doctor talks to the patient To raise medical history (Anamnese). The doctor inquires about the general health of the patient. He also asks if there are any complaints or restrictions in everyday life. These include, for example, back pain, difficulty climbing stairs, lifting heavy objects or pain during long running.
Also important to the doctor is information about possible fractures or falls in the past. In addition, the doctor asks if the patient suffers from a disease or uses medication.
Physical examination
This is followed by a physical examination. The doctor also measures the height and weight of the patient.
Tests are used to check physical fitness and mobility. An example is the “timed-up-and-go” procedure:
At the same time, the doctor stops the time it takes the patient to get up from a chair, walk three meters, turn around, go back and sit down again. He may also use any walking aids that he otherwise uses in everyday life.
If the patient needs more than 30 seconds for the task, he is likely to be impaired in his mobility. Then there is an increased risk of falling.
Measurement of bone density
Another important component of osteoporosis diagnostics is the Bone density measurement (osteodensitometry, DXA measurement), Low-dose X-rays are used to determine the bone density on the lumbar spine, the entire thighbone and the thighbone. The measured values (T values) are compared with the typical mean values in the respective age group. If they are 2.5 units or more below the age-typical averages, the osteoporosis definition is fulfilled: the patient has bone loss.
Overall, the World Health Organization (WHO) distinguishes bone density measurement depending on the T-value four stages of bone loss:
- Grade 0: Osteopenia. In this precursor of osteoporosis, the mineral content of the bones is reduced by a value of 1 to 2.5.
- Grade 1: Osteoporosis. The mineral content of the bones is reduced by more than 2.5. Broken bones (fractures) are not yet available.
- Grade 2: Manifest Osteoporosis. It occurs when the bone mineral content is reduced by more than 2.5, and the patient already had one to three vertebral fractures.
- Grade 3: advanced osteoporosis. All patients with bone mineral content greater than 2.5 units below average and multiple (multiple) vertebral body fractures have advanced osteoporosis.
X-ray
Possible fractures (fractures) can be detected on an x-ray. Osteoporosis often causes vertebral body fractures. They can be caused by a single event (such as a fall) or can be the result of long-lasting, subtle mechanical effects.
The second case is creeping fractures. They cause the vertebral body in question to deform. Experts call this as Sintering or creep deformation, The stronger the deformations, the more pronounced the osteoporosis. This can be determined by measuring the vertebral body heights between the fourth thoracic vertebrae and the fifth lumbar vertebrae by means of X-rays. The obtained measured value (Wirbeldeformitätsscore) indicates how pronounced osteoporosis is.
blood tests
In the context of osteoporosis diagnostics, the patient’s blood is also examined. On the one hand, a blood picture is created. In addition, other parameters are determined, such as liver and kidney values and calcium and phosphate levels. The main purpose of the investigation is to clarify possible causes of secondary osteoporosis.
In addition, the blood levels help the doctor in the treatment planning: For example, if the calcium level in the blood is very low, the patient must not be treated with certain drugs of osteoporosis.
Osteoporosis basic diagnostics: For whom recommended?
In all people with an increased bone fracture risk, an osteoporosis basic diagnosis should be carried out. These risk groups generally count Women and men from the age of 70 years.
An osteoporosis investigation is also recommended People over 50 years at various risk factors for osteoporosis-related fractures. These include, for example:
- Vertebral fractures after trivial injuries (like falling out of state)
- Hip-thigh fracture in mother or father
- Immobility, such as prolonged bed rest or cast after surgery or accidents
- Underweight (body mass index below 20), weight loss and anorexia (anorexia nervosa)
- Smoking and chronic obstructive pulmonary disease (COPD)
- high alcohol consumption
- hormone-related diseases such as Cushing’s syndrome, hyperthyroidism, growth hormone deficiency due to a pituitary dysfunction (pituitary gland), diabetes mellitus (Type 1 and Type 2 diabetes mellitus)
- rheumatologic diseases (rheumatoid arthritis, systemic lupus erythematosus, ankylosing spondylitis)
- Gastrointestinal diseases such as celiac disease, even stomach surgery (complete or partial removal of the stomach)
- neurological / psychiatric disorders such as epilepsy, schizophrenia, Alzheimer’s, Parkinson’s, stroke, depression
- Heart failure (heart failure)
- alcohol-related liver diseases
- certain medications such as high-dose cortisone, anticonvulsants, antidepressants, glitazones (for type 2 diabetes), aromatase inhibitors (for breast cancer), prostate cancer for anti-hormone treatment, opioids (strong painkillers)
Further investigations
Outside of osteoporosis basic diagnostics, the doctor may in some cases carry out further examinations. For example, sometimes a computed tomography (CT) or magnetic resonance imaging (MRI) is needed to rule out other possible causes of patient discomfort. These imaging techniques may also be important for therapy planning, such as when a fracture first needs to be clarified.
In rare cases, the doctor takes a sample of the bone tissue (bone biopsy). It is examined more closely in the laboratory. This can be helpful, for example, if the other examinations have yielded only an unclear finding.
Osteoporosis: treatment
Osteoporosis therapy consists of several building blocks. It is individually adapted to the patient. Among other things, the doctor takes into account in the planning of therapy, whereby the bone loss was triggered and how pronounced he is.
General information on osteoporosis therapy
Among the most important basic measures of any osteoporosis therapy count adequate exercise and the right nutrition, If necessary, the patient receives additional medication against the bone loss.
Also important is one fall prevention: Osteoporosis patients easily break bones. Here are some tips to reduce the risk of falls and accidents:
- The apartment should be sufficiently lit and furnished so that you can not easily stumble and fall. For example, remove tripping hazards such as slipping carpets and exposed cables.
- If the eyes wane, patients should wear a suitable visual aid.
- High-heeled shoes and those with smooth soles are unsuitable. Ratsamer are flat shoes with non-slip soles.
- If possible, osteoporosis patients should not take any medication that restricts attention and responsiveness. These include sleeping pills, allergy remedies and antidepressants.
In secondary osteoporosis as a result of another disease (such as hyperthyroidism) you have this Treat underlying disease, Otherwise, osteoporosis therapy may not bring the desired results.
If certain medications have triggered a secondary osteoporosis, one should try as possible “bone-friendly” preparations switch to medication that has less negative impact on bone density. This is recommended, for example, in women who are being treated with glitazones because of type 2 diabetes.
Exercise as osteoporosis therapy
With regular exercise, you can both prevent and treat bone loss. It is very important to choose the right form of exercise or sport.
First thing is: in osteoporosis therapy is no competitive sports necessary! For example, efficient osteoporosis treatment starts with you walk regularly walk. This promotes bone formation and inhibits bone resorption. Also easy running training like jogging or walking are very effective.
swim is also recommended as an osteoporosis therapy. Twice a week half an hour back or breaststroke are ideal. There are also other muscle groups trained than walking, for example, the back muscles.
Also water aerobics and light weight training are suitable for the treatment of osteoporosis. gymnastics outside the swimming pool as well as simple Osteoporosis exercises You can do it independently at home. Here too, you can already achieve good effects twice a week with a half-hour training session. Tips for suitable exercises can be obtained, for example, from the doctor, sports physician or in a special sports group for osteoporosis patients.
As a general rule: Discuss with your doctor which type of exercise and / or sport and what intensity of exercise is most appropriate in your case.
Diet as osteoporosis therapy
To each osteoporosis therapy belongs – in addition to sufficient exercise – the right diet. Here are the most important tips:
Eat well. Make sure that your body with sufficient calcium supply. The mineral is important for healthy, strong bones. Per day, adults should provide their body with the diet with 1,000 milligrams of calcium. It is mainly found in dairy products, but is also found in green vegetables such as spinach and broccoli, as well as in some mineral water types. Some foods also contain calcium, such as juices.
Some patients can not be sure that they are getting enough calcium through their diet. Then the doctor prescribes additionally Calcium supplements (for example effervescent tablets).
In addition to calcium is too Vitamin D Very important for osteoporosis patients (and other people): It ensures that the body can pick up calcium from the gut and build it into the bones. Good dietary sources of vitamin D are fatty fish, eggs, butter and milk.
In addition, you should regularly expose the skin to sunlight: With the help of UV light, the body can produce vitamin D itself. With this in-house production, he even covers most of his needs. In summer you should spend 5 to 15 minutes daily in the sun, in spring and autumn 10 to 25 minutes. It is enough to let your face and hands be “irradiated”. Depending on the temperature you can let the suns act on the uncovered arms and legs.
Often doctors prescribe for osteoporosis as well Vitamin D supplements, This should ensure the supply. Such preparations are particularly useful in patients at high risk for falls or broken bones, which are exposed to little sunlight. The daily dose is 800 to 1,000 International Units (IU) of vitamin D3.
It also takes for solid bones phosphate, but in the right proportion to the calcium intake. An excess of phosphate binds calcium so that it can no longer be incorporated into the bones. You should therefore avoid phosphate-rich foods and drinks such as meat, sausage, processed cheese and cola drinks.
Phosphates can be recognized in the list of ingredients on food and beverage packages at numbers E 338-341 and E 450.
Medicines for osteoporosis
If osteoporosis patients are at high risk for fractures, the doctor prescribes in addition a drug therapy osteoporosis. The following active ingredients are available:
- bisphosphonates: Bisphosphonates such as alendronate and zoledronate are the first choice in osteoporosis therapy. They prevent excessive bone loss and strengthen the remaining bone mass. Bisphosphonates are taken in tablet form daily, weekly or monthly or administered by syringe or infusion.
- Selective Estrogen Receptor Modulators (SERM): For osteoporosis therapy, the representative raloxifene is approved for this group of active substances. It binds to specific docking sites (receptors) that are actually intended for estrogens, thus inhibiting bone resorption. Raloxifene is taken daily as a tablet.
- Protelos: This drug also inhibits bone resorption and also increases the activity of bone building cells. It is taken daily as a powder solution.
- teriparatide: Teriparatide is a derivative of the body’s hormone parathyroid hormone. It promotes bone formation and the formation of new bone structures. The drug is injected once daily under the skin.
- denosumab: Denosumab is a so-called monoclonal antibody. It intervenes in the bone metabolism and inhibits the bone-degrading cells (osteoclasts). Denosumab is given as a syringe under the skin.
In individual cases, other drugs for osteoporosis therapy can be used such as female sex hormones or calcitonin.
pain Management
Against the pain in osteoporosis, the doctor can initiate a suitable pain therapy. Often Painkiller from the group of non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, acetylsalicylic acid (ASA) or diclofenac. In case of severe pain, the doctor may also prescribe so-called opiates. In some cases, other drugs are useful, for example Muscle-relaxing drugs (Muscle relaxants).
Physical therapy measures often help against osteoporotic pain. These include, for example Cold or heat treatments, massages or acupuncture, In some patients, the symptoms can be sufficiently alleviated. For others, physical therapies can supplement the treatment with painkillers.
For prolonged pain due to vertebral body fractures, the doctor may also prescribe a semi-elastic bodice to the patient.
surgery
at Vertebral collapses a surgical intervention may be useful. In the so-called vertebroplasty The surgeon inserts bone cement into the fractured vertebral body. This is stabilized thereby. At a kyphoplasty the vertebral body is first inflated with a small balloon. This can raise the bone a bit and also facilitates the introduction of cement.
Other fractures due to osteoporosis also sometimes require surgery. For example, some patients get an artificial hip joint after a femoral neck fracture.
More tips on osteoporosis therapy
- Avoid underweight.
- Avoid nicotine and alcohol.
- Take care in everyday life to a back-friendly behavior (for example, upright sitting position, regular change of posture, no carrying heavy loads, no stooping posture at the housework, replacing worn mattresses).
It is also helpful to join a support group for osteoporosis patients. Such groups offer advice, help and exchange with other patients. Take advantage of this offer if you have the opportunity!
Osteoporosis: disease course and prognosis
Osteoporosis is not curable so far. It is all the more important to recognize and treat them as early as possible. Without treatment osteoporosis progresses. Patients are increasingly suffering from bone pain (such as back or neck pain). The fractures pile up. Especially in old age, many people can not recover from heavier fractures.
Especially feared is the femoral neck fracture. He may cause serious complications and sequelae such as rebleeding and wound healing disorders. The necessary surgery (such as the use of an artificial hip joint) carries further risks for those affected. Many of the older patients are then only limited mobility or even become a nursing case. About 10 to 20 percent of patients with femoral neck fracture die from complications or surgical risks.
Osteoporosis: prevention
Those who want to prevent osteoporosis should minimize the known risk factors. These include, for example, lack of exercise as well as a lack of calcium and vitamin D. Here are the key tips:
- Look for a calcium-rich diet with dairy and calcium-containing water. Adults should take in 1,000 to 1,500 milligrams of calcium per day.
- Regularly eat products with high levels of vitamin D, such as fatty fish (such as herring), fish oil and egg yolk.
- Exposure face and hands (and other exposed areas, if possible) regularly to sunlight: five to fifteen minutes daily in summer, ten to twenty-five minutes daily in spring and autumn. Then the body can cover most of its vitamin D needs by making the vitamin itself.
- Avoid foods that contain a lot of phosphate. They inhibit calcium uptake in the gut and promote calcium release from the bones. Meat and sausage products, processed cheese and cola drinks, for example, are rich in phosphate.
- Avoid tobacco and alcohol and do not drink too much coffee. These stimulants are also bad for the bones.
- Another indispensable component of the osteoporosisPrevention is regular exercise. Be physically active regularly, preferably several times a week. This strengthens the bones.
Weiterführende Informationen
Leitlinien:
- Leitlinie “Prophylaxe, Diagnostik und Therapie der Osteoporose” des Dachverbands der Deutschsprachigen Wissenschaftlichen Osteologischen Gesellschaften e.V. (2017)
Selbsthilfegruppen:
- Osteoporose Selbsthilfegruppen Dachverband e.V.