Pancreatic cancer is treacherous: for a long time the disease remains asymptomatic. Later, the symptoms are similar to those of a chronically inflamed pancreas (upper abdominal pain, indigestion, etc.). Therefore, pancreatic cancer is often only discovered when it is already advanced. The chances of recovery are then usually bad. Read what symptoms of pancreatic cancer can occur, how the tumor is formed and treated, and what the prognosis is!
Quick Overview
- What is pancreatic cancer? Malignant tumor of the pancreas. Is relatively rare in Germany (about 16 out of every 100,000 people get sick every year). The mean age of onset is 70 years (men) and 76 years (women). Despite its rarity, pancreatic carcinoma is the third most common tumor of the gastrointestinal tract (after bowel and stomach cancer).
- Risk factors: Smoking, alcohol consumption, obesity, diabetes (diabetes mellitus), hereditary breast cancer or ovarian cancer etc.
- symptoms: no complaints for a long time; later upper abdominal pain, back pain, weight loss, loss of appetite, jaundice, diabetes mellitus, nausea and vomiting, indigestion, fatty stool etc.
- investigations: Blood tests (with determination of tumor markers), abdominal ultrasound, endoscopic ultrasound (endosonography), computed tomography (CT), magnetic resonance imaging (MRI), magnetic resonance cholangiopancreatography (MRCP), removal and analysis of a tissue sample, possibly laparoscopy ( Laparoscopy), chest X-ray (chest radiograph) and further examinations
- Treatment: Surgery, if necessary chemotherapy, radiotherapy (only in certain cases), pain therapy
- Forecast: Healing only possible if the tumor is still localized. However, because pancreatic cancer is often discovered late and usually grows rapidly and aggressively, the prognosis is generally unfavorable.
Pancreatic cancer: symptoms
The pancreatic cancer symptoms are recognized by the Type and location of the tumor affected:
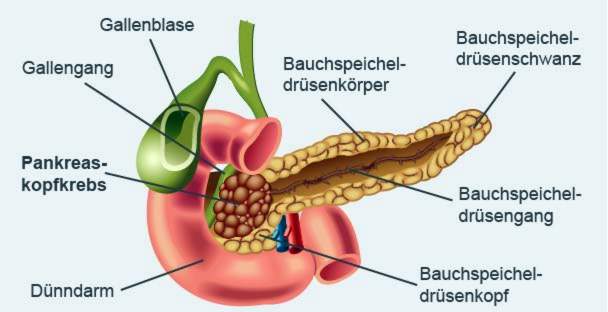
The pancreas consisting of head, body and tail parts (medical pancreas) lies in the upper abdomen behind the stomach and immediately in front of the spine. It consists of two different types of glandular tissue:
- The largest part is the exocrine tissue, It produces an enzyme-containing digestive juice that is channeled into the small intestine.
- Scattered into the exocrine glandular tissue are cell groups of endocrine tissue, the so-called Langerhans Islands. These glandular cells produce hormones such as the hypoglycemic insulin and its antagonist glucagon. They are released into the blood.
Approximately 95 percent All tumors of the pancreas develop from the exocrine glandular tissue, In the remaining cases, the tumor is produced by hormone-forming (endocrine) glandular cells. Depending on the type of cell, one speaks for example of an insulinoma or a glucagonom.
The most common is pancreatic cancer in the head of the pancreas.
Common symptoms of pancreatic cancer
For many types of pancreatic carcinoma, sufferers usually do not notice the disease for a long time. As soon as symptoms appear, the cancerous tumor often presses on or even grows into neighboring structures (bile duct, stomach, small intestine, etc.). Not infrequently there are already daughter abductions (metastases). Often, at this advanced stage of pancreatic cancer, symptoms of the following kind occur:
- persistent pain in the upper abdomen and back: The back pain can increase in the supine position.
- loss of appetite
- Weight loss: If pancreatic cancer causes exocrine tissue to produce too little or no digestive enzymes, the nutrients in the intestine can only be reduced to a limited extent or not at all. The impaired nutrient supply leads to weight loss.
- Indigestion and fat stool: The lack of digestive enzymes from the diseased pancreas causes, among other things, that the fat from the food in the gut can no longer be properly absorbed. It is then excreted undigested with the stool – the resulting fat stool is bright, shiny and has a pungent odor.
- Nausea and vomiting
- Jaundice (jaundice): Pancreatic cancer in the pancreatic head may press on the bile duct or close it (it runs a little way through the pancreatic head). The bile then accumulates, which causes jaundice: skin, mucous membranes and the white dermis in the eye turn yellowish. The urine is dark, the chair is light.
- Diabetes (diabetes mellitus): Sometimes the tumor produces too little or no insulin. It is then usually an endocrine tumor. Insulin deficiency leads to diabetes.
The symptoms of pancreatic cancer are similar to those of pancreatitis (pancreatitis). Sometimes both diseases occur together. Both can make the diagnosis more difficult.
An endocrine pancreatic tumor sometimes produces more of the stomach acid stimulating hormone gastrin. That can lead to the formation of a stomach ulcers because too much stomach acid causes severe irritation to the gastric mucosa. Since gastric ulcers can have other causes, they are just as rare among the specific symptoms of pancreatic cancer as back pain.
Rarely, small pancreatic clots form in pancreatic cancer due to pressure on surrounding vessels. These can clog the affected vessel (thrombosis). This often happens, for example, in the splenic vein, which runs near the pancreas.
The pancreas also contains a high concentration of the blood coagulation factor thrombokinase. The cancerous organ changes can disrupt the blood clotting system, causing small clots to form throughout the vessels (disseminated intravascular coagulopathy, DIC). The coagulation factors are thereby used up, which increases the risk of bleeding. In addition, clots may peel off and clog a vessel elsewhere (embolism).
If the pancreatic cancer spreads to the peritoneum (peritoneal carcinosis), but the cancer cells fluid into the abdominal cavity – it creates a “Ascites“(Ascites). Possible signs include a bulging or enlarged stomach, unwanted weight gain and indigestion.
Pancreatic cancer: treatment
An early discovered pancreatic carcinoma tries to heal as completely as possible. Unfortunately, however, pancreatic cancer is often discovered very late. A cure is then usually no longer possible. The treatment then serves to alleviate the patients’ complaints and to slow down or stop further spread of the tumor (palliative therapy).
In principle, the doctor has various options for pancreatic cancer treatment available. When which therapy makes sense depends on the individual case.
Operative therapy
Surgery is only an option in 10 to 20 percent of patients with pancreatic cancer. The procedure only really brings something if the surrounding tissue is still cancer-free. If the tumor can be completely removed during the operation, healing may be possible.
Most commonly, pancreatic cancer develops in the pancreatic head. Then, in general, one Kausch-Whipple operation The surgeon removes the pancreatic head, gallbladder, bile duct, small intestine, lower stomach and regional lymph nodes. An alternative is the pylorus-preserving pancreatic head resection, The lower part of the stomach (pylorus = stomach outlet) is preserved.
In the case of pancreatic carcinoma in the tail of the pancreas, the spleen often has to be removed as well.
In some cases of pancreatic cancer, it is not enough to excise the diseased tissue from the pancreas – it must whole pancreas removed become.
After the surgery, many patients need the missing ones Pancreatic digestive enzymes in capsule form taking. Only then can digestion continue to function.
chemotherapy
As a rule, the pancreatic cancer surgery is followed by chemotherapy (adjuvant chemotherapy). Special medicines (cytostatics) are administered which can prevent the rapid division of cells. This is how cancer cells, which may still be present in the body after the operation, should be eliminated. If possible, chemotherapy should be started within six weeks of surgery and last half a year.
Sometimes chemotherapy is done before the operation. These Neoadjuvant chemotherapy should reduce the size of the tumor so that it will be easier to excise.
radiotherapy
Radiation therapy (radiotherapy) for pancreatic cancer is not generally recommended. However, it can be used in controlled trials. For example, in such a study, one can try to support the treatment of pancreatic cancer with combined radiotherapy and chemotherapy (chemoradiotherapy). This can be considered for a locally advanced pancreatic carcinoma, which can not be operated on successfully.
In the case of an incurable pancreatic cancer, radiation can also be used specifically to relieve symptoms (such as cancer pain).
pain Management
Many people with pancreatic cancer suffer from severe abdominal pain. These are treated by means of a pain therapy after the Stages of the World Health Organization (WHO):
First, one tries to relieve the pain with non-opioid-containing agents such as acetaminophen or ASA. If this is not enough, the doctor also prescribes weakly effective opioids such as tramadol. If the pain can not be controlled, the non-opioid painkillers of stage 1 are combined with potent opioids (such as morphine). These have the strongest analgesic effect.
In some patients with no longer curable pancreatic cancer, this drug therapy does not help enough. Then you can try one Block the nerves in the stomach, the so-called celiac plexus. This prevents the transmission of pain stimuli to the brain.
Other measures
Particularly in the palliative treatment of pancreatic cancer (ie in the case of no longer curable cancer), further measures are often taken for the well-being of the patient. One wants to achieve that the patient can spend his remaining lifetime as possible without (strong) complaints.
This can often be achieved with a customized pain therapy (as described above). If necessary, additional palliative measures are added. For example, if the tumor narrows or obstructs the bile duct, sufferers suffer from jaundice. Then one can endoscopic procedure help: Using a thin, tubular instrument (endoscope), the doctor introduces a small plastic tube (stent) into the bile duct to keep it open.
Also by means of an endoscope can be widened by the tumor einenter stomach outlet. In the case of severe constriction, it may make sense to provide the patient with the necessary nutrients via a feeding tube in the future (enteral nutrition). Also possible is one parenteral nutrition – the administration of nutrient solutions directly into the blood.
In addition to physicians, physiotherapists, masseurs, social workers, psychologists and counselors can effectively support the palliative treatment of pancreatic cancer patients.
For all palliative therapies for pancreatic cancer, the doctor and the patient must jointly consider that the mean life expectancy for inoperable tumors is only three to five months after diagnosis. Therefore, measures that cause serious side effects should be avoided here.
Nutrition in pancreatic cancer
There are no specific dietary requirements for pancreatic cancer. Patients should eat what they tolerate best. Generally, however easily digestible food recommended. It should be divided into several small meals instead of the usual three main meals per day. The fat intake should be limited. Even hard-to-digest dietary fiber such as raw food or whole grains should end up on the plate too often. Alcohol should be taboo in pancreatic cancer.
To compensate for the defective digestive function in pancreatic cancer, the corresponding enzymes in the form of a substitution preparation (pancreatin) can be supplied. The patient takes the pancreatin capsules with the meal.
Pancreatic cancer: causes and risk factors
At present, it is not completely clear why pancreatic cancer develops. Probably one plays hereditary predisposition a certain role. Smoke and alcohol consumption are considered as assured risk factors: According to experts, the so-called cotinine level is increased in heavy smokers. This substance is produced by the breakdown of nicotine in the body and is considered carcinogenic. With regular alcohol consumption, the pancreas often inflames – and chronic inflammation makes the glandular tissue more susceptible to pancreatic cancer.
The metabolism changes can also contribute to a kind of chronic inflammation heavy overweight and belly fat to lead. That’s why obese people are more likely to contract pancreatic cancer. There at Diabetes mellitusPatients with pancreatic tissue are also predisposed to pancreatic cancer.
Certain diseases are other assured risk factors. So have women with hereditary breast cancer or ovarian cancer as well as their relatives an increased risk for pancreatic carcinoma. Some rare hereditary diseases also make them more susceptible to a malignant pancreatic tumor (e.g., Peutz-Jeghers syndrome).
In addition, there are some factors that are thought to increase the risk of pancreatic cancer. These include frequent consumption of sugar and smoked or grilled foods and frequent contact with certain chemicals and toxins (chromium and chromium compounds, chlorinated hydrocarbons, herbicides, pesticides, etc.).
Tip: To reduce the risk of pancreatic cancer, you should not smoke, avoid alcohol as far as possible and pay attention to a healthy body weight. A diet rich in fruits and vegetables may also reduce the risk of illness.
Pancreatic cancer: examinations and diagnosis
In case of suspected pancreatic cancer, the doctor will first have a detailed conversation with the patient in order to avoid it To raise medical history (Anamnese). Among other things, he can describe all the complaints exactly, asking for possible pre-existing conditions and for known pancreatic carcinoma disorders in the family.
Follow after the anamnesis interview various investigations, They serve to clarify the suspected pancreatic cancer and to exclude diseases with similar symptoms (such as pancreatitis). If confirmed suspected pancreatic carcinoma, the investigations also help to determine the spread of the tumor in the body.
- Physical examination: For example, the doctor scans the abdomen to detect swelling or induration in the abdomen.
- Blood test: A blood analysis gives the physician information about the general state of health of the patient as well as the function of various organs (such as the liver). In addition, so-called tumor markers are determined. These are certain substances that may be elevated in a tumor disease (CA 19-9, CA 50, CEA). Based on the tumor markers, the tumor stage can be determined and the course of the disease can be assessed.
- Abdominal ultrasound: Using ultrasound, the physician can assess the size and condition of the pancreas and other abdominal organs (liver, gall bladder, stomach, small intestine, etc.) and the surrounding lymph nodes.
- Endoscopic ultrasound: This is an endoscopic ultrasound examination (ultrasound “from the inside”). A tubular instrument (endoscope) is pushed over the mouth and stomach into the duodenum with a small ultrasound probe. Since the pancreas is close to it, even the smallest tissue changes can be detected in the ultrasound. If necessary, the doctor can also insert a fine hollow needle into the interior via the endoscope in order to remove a tissue sample from the pancreas (biopsy).
- Tissue sample: As mentioned, tissue samples from suspicious sites are usually taken during endosonography. But you can also introduce a hollow needle directly over the abdominal wall in the pancreas to remove tissue.
- Computed Tomography (CT): With this special X-ray examination, detailed sectional images of the pancreas and other structures are made. This allows the doctor to assess the exact location and size of the tumor and to detect possible dislocations (such as in lymph nodes or liver).
- Magnetic Resonance Imaging (MRI): Again, detailed cross-sectional images of body structures are made, but with the help of strong electromagnetic fields. The location and spread (metastases) of the cancer can be easily recognized. Particularly meaningful with regard to a pancreatic cancer diagnosis is the Magnetic Resonance Cholangiopancreatography (MRCP): In this MRI scan, the ductwork of the pancreas and gallbladder are shown in detail. Most pancreatic carcinomas develop from the cells lining excretory ducts of the exocrine glandular tissue (so-called adenocarcinomas).
- Laparoscopy: Sometimes there are indications that the pancreatic tumor has already spread to neighboring organs or to the peritoneum (for example with a markedly elevated tumor marker CA 19-9 or ascites), although no metastases can be detected in the imaging. Then a laparoscopy can bring clarity.
- Chest X-ray: X-ray images reveal any secondary tumors (metastases) in the lungs.
Pancreatic Carcinoma: Stages
Depending on the extent of malignant tissue alteration, pancreatic cancer is divided into four stages:
- Stage 1: The tumor is limited to the pancreas.
- Stage 2: The adjacent tissue is also affected by the cancer.
- Stage 3: There are metastases in the lymphatic tissue.
- Stage 4: Metastases have also formed in other organs (such as lung or liver metastases).
Pancreatic cancer: disease course and prognosis
The course of disease in pancreatic cancer depends mainly on the Type of tumor ab: Most pancreatic carcinomas are adenocarcinomas (originated from the cells lining the excretory ducts of the exocrine glandular tissue). These tumors grow rapidly and spread rapidly through blood and lymph into other parts of the body. If they are not detected early (which is rarely the case), the Prognosis rather unfavorable out. Rarer forms of pancreatic cancer, however, usually grow slower and less aggressive. Your prognosis is therefore usually cheaper.
In general, the sooner a pancreatic carcinoma is detected and treated, the better the chance of recovery. If the tumor is not operable, it is Life expectancy low: On average, those affected die three to four months after the diagnosis.
Overall, the pancreatic cancer shows the lowest survival rates of all cancers Five years after diagnosis, only nine to ten percent of patients have not yet died from the pancreatic tumor (relative five-year survival rate for Germany).
Additional information
Books:
- Pancreatic cancer: advice and help for those affected and relatives (advice and help) by Hermann Delbrück, Kohlhammer, 2010
guidelines:
- Guideline “exocrine pancreatic carcinoma” of the German Cancer Society and the German Society for Gastroenterology, Digestive and Metabolic Diseases (2013)
- Patient Guideline “Cancer of the Pancreas” of the German Cancer Society and the German Society for Gastroenterology, Digestive and Metabolic Diseases (2014)
Self-help:
- The working group of pancreatectomy e. V.
- The German Pancreatic Club e.V.
- TEB e.V. self-help
- Pancreatic Cancer Center