A bipolar disorder is a serious mental illness. People who suffer from it experience a constant ups and downs of emotions. At times, the affected feel very depressed, then again they are euphoric, turned on, hyperactive and overestimate themselves. Read how to recognize bipolar disorder and how to treat it.

Quick Overview
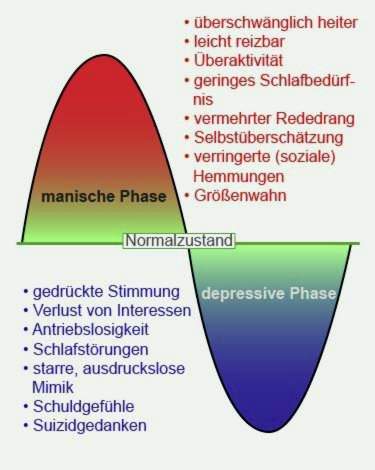
symptoms: Change between depressive symptoms and phases of exaggerated elation, risk behavior, megalomania, isolated hallucinations
Causes: highly genetically predisposed, disturbance of messenger balance in the brain, stress, certain medications
Diagnosis: Diagnosis based on symptoms is often confused with classic depression or schizophrenia
Treatment: Medication, psychotherapy, watch therapy, electroconvulsive therapy, therapy often difficult because of lack of insight
Forecast: hardly curable, stabilized by drugs, high risk of suicide, therefore early therapy important
Bipolar disorder: description
Bipolar disorder, like depression, is one of the so-called affective disorders. This means that it affects the feelings of those affected. You experience strong mood swings, for which there is usually no external trigger. Manic phases with great euphoria, energy and self-overestimation suddenly change in depressive phases in which the affected are depressed and unpowered. Often the bipolar disorder is therefore still colloquially referred to as Manic Depression.
Bipolar Disorder: The Different Forms
In a bipolar disorder, phases of mania and depression alternate. In some patients, however, several months or even years may be between depressive and manic episodes. In between, their mood is balanced. About 20 percent of sufferers experience exclusively manic and no depressive phases.
The bipolar disorder is divided into the following forms:
- Bipolar I disorder: alternately occurring depressive and manic phases
- Bipolar II Disorder: alternately occurring depressive and mildly manic (hypomanic) phases
- Cyclothymia: alternately occurring depressive and manic phases in a strongly attenuated form
Bipolar disorder: symptoms
In more than half of manic-depressive patients, the disease begins with a depressive phase. Later in the process, manic or hypomanic (mildly manic) phases occur.
Symptoms in the depressive phase
In the depressive phases, the clinical picture is similar to depression. The main symptoms then belong
- Gloomy mood
- Loss of interest and joy
- listlessness
- Sleep disorders, especially during sleep disturbances in the second half of the night
- Concentration and thought disorders
- guilt
- self-doubt
- suicidal thoughts
External symptoms
Facial facial expression tends to be rigid and expressionless during depressive episodes. Those affected usually speak quietly and their answers are delayed.
Physical symptoms
In the depressive phase also physical symptoms can occur. The appetite decreases, and many sufferers lose significant weight. Some feel pain in different parts of the body. Common symptoms include respiratory distress, heart problems, stomach and intestinal problems, dizziness, headache and erectile dysfunction.
Bipolar disorder: symptoms in the manic phase
In phases of mania, the previously depressive mood completely reverses. This phase is not always easy to see at first. Often sufferers are initially only more active and positive mood than in the depressive phase. It may also remain with this weakened manifestation of mania. This is called hypomania.
overactivity
The good mood can also take on extreme proportions. Without cause, manic-depressive are exuberantly cheerful or even irritated. Typical signs are also overactivity, a reduced need for sleep and an increased need for speech.
Overconfidence and carelessness
What is dangerous about the mania is that those affected lose their relationship to reality. They tend to overconfidence and reckless behavior. They spend money without hesitation and start oversized projects that can lead to financial and legal problems.
Another problem is that social inhibitions are lost. Affected then arbitrarily approach strangers and tend to a more open flirtation and sexual behavior.
Megalomania
If excessive self-esteem becomes megalomania and hallucinations occur, it is a mania with psychotic symptoms. Affected then believe, for example, have great skills, to become famous or to change the world.
Creative potential
People with bipolar disorder are often very creative. Today, it is believed that Vincent van Gogh and Georg Friedrich Händel, among others, were manic-depressive.
Bipolar disorder: mixed phase symptoms
The mixed phase of bipolar disorder is when both depressive and manic symptoms occur simultaneously or within a very short time. The mood then changes from sad to euphoric and happy or vice versa. This emotional roller coaster is hard to bear.
suicide risk
This form of bipolar disorder is associated with great suffering. The danger of suicide is great: Negative thoughts and feelings make those affected despair, at the same time the manic energy drives them on. This dangerous constellation can cause them to put their suicidal thoughts into action on impulse.
Bipolar disorder: Mental illnesses
Frequently, in addition to the bipolar disorder, further mental problems occur. Manic-depressants most commonly suffer from anxiety disorders or a personality disorder.
Many patients are substance dependent. Consumption of alcohol or drugs worsens the course of the disease. The treatment of such comorbidities is necessary for a successful therapy of bipolar disorder. Otherwise symptoms of concomitant diseases can adversely affect the course of the disease.
Bipolar disorder: causes and risk factors
Bipolar disorder is caused by both biological and psychosocial factors. Previous studies suggest that a complicated interaction of several genes with different environmental factors favors the disease.
Bipolar Disorder: Genetic Causes
Family and twin studies have shown that genetic factors are involved in the development of Bipolar Disorder. Thus, children of a sick parent with ten percent probability also manic-depressive. If there is a bipolar disorder in both parents, the probability of disease increases even up to 50 percent.
So far, however, no specific gene for the manic-depressive disease was found. Presumably, several genes are involved in a bipolar disorder.
Bipolar disorder: influence of neurotransmitters
There are many indications that bipolar disorder disturbs the distribution and regulation of important messenger substances (neurotransmitters) in the brain. Neurotransmitters are endogenous substances that cause certain reactions in the body and in the brain. Examples are serotonin, norepinephrine or dopamine.
Depressed people have been diagnosed with norepinephrine and serotonin deficiency. In manic phases, however, the concentration of dopamine and norepinephrine is increased. In bipolar disorder, therefore, the imbalance of the various messengers may play an important role. The medical treatment of bipolar disorder therefore aims to achieve a controlled release of these signaling substances.
Bipolar Disorder: Psychosocial Causes
In addition to the biological influences, the individual circumstances of life are also involved in a bipolar disorder. Especially stress seems to be a trigger for manic-depressive episodes.
Severe illnesses, bullying or separations, but also some phases of life such as puberty, mean a longer stress phase. How stress is felt and processed depends on the individual. Some people have developed good strategies to deal with stress while others are quickly overwhelmed.
Stress can have been a bad childhood event or a recent divorce or the death of a loved one. Such stress-inducing factors increase the likelihood of getting bipolar disorder.
Bipolar disorder: drug-related causes
Even some medications can change the mood and in extreme cases trigger a bipolar disorder. These include cortisone drugs, methylphenidate, certain antiparkinsonian and epilepsy drugs, but also drugs like alcohol, LSD, marijuana and cocaine. There are also individual case reports, according to which Bipolar Disorders after Brain Injuries should have occurred.
Bipolar disorder: examinations and diagnosis
Bipolar disorder is not easy to diagnose because it can be confused with other mental disorders such as classic depression or schizophrenia. Since the manic phase is often interpreted by the relatives and sufferers as a mere fuss, it often takes years before a correct diagnosis is made.
In particular, the bipolar II disorder and the cyclothymia are difficult to recognize, since the symptoms are weaker here than in the bipolar I disorder. It is therefore particularly important to describe to the doctor or therapist experience, moods and feelings in detail.
If a bipolar disorder is suspected, the family doctor can be contacted first. Due to the difficult diagnosis and the increased risk of suicide, it is advisable to immediately contact a clinic or consult a specialist in psychiatry. Often, however, sufferers see no need for medical help – especially during their manic phase.
If you persuade yourself to visit a doctor, it makes sense to ask the family members as well. If the person concerned does not have an insight into the illness, the observations of related persons are very helpful for the diagnosis “bipolar disorder”. So relatives can often assess the different mood phases well.
The diagnosis Bipolar Disorder is made using special clinical questionnaires. The following questions could ask the doctor or therapist in a first interview:
- Have you felt depressed or driftless in the last few weeks?
- Did you have trouble getting up in the morning?
- Did you have trouble sleeping through the night?
- Did you have a good appetite?
- What are your thoughts at the moment? What is your concern?
- Do you sometimes have thoughts about death or about taking your own life?
- Have you been unusually upset in the last few weeks?
- Did you have the feeling that you are under power?
- Did you get the impression that you talked more and faster than usual?
- Was your need for sleep reduced?
- Were you very active and did many things in no time?
- Has your mood been changing lately?
Due to the large genetic influence, a family history is very useful in manic-depressive illness. This allows the therapist to find out if other members of the family are suffering from bipolar disorder.
Bipolar disorder: treatment
The diagnosis “bipolar disorder” urgently requires the intake of medication. The drugs not only reduce the depressive and manic phases, they also reduce the risk of suicide.
Psychotherapeutic treatment is just as important as drug therapy. It can positively influence the course of bipolar disorder. Above all, it is crucial for the insight into illness and the will to be treated. This so-called compliance is often missing people with bipolar disorder, because they feel particularly good in the manic phases and reluctant to do without. Manic-depressives usually have to be treated for a lifetime, because only then can the mood be kept stable. If patients stop treatment, there is a high risk of relapse.
Bipolar Disorder: Phases of Treatment
The treatment itself consists of an acute treatment, stabilization phase and relapse prevention.
Acute phase
In the acute phase, especially drugs are used to treat the onset of mania or depression.
For psychological support, therapeutic discussions are offered in individual or group therapy. Some clinics also use wakefulness and electroconvulsive therapies to normalize mood.
stabilization phase
It may take a few weeks or even months for a significant improvement in symptoms to occur. Then the stabilization phase begins. The drugs are adjusted during this phase until the patient receives the optimal dosage for him.
Relapse prevention
If the affected person then largely symptom-free, one tries to maintain this condition in the long term. For this it is necessary that the patient continues to take medication. In addition, he learns in therapy to recognize the warning signs of mania or depression early, and can counteract.
Bipolar disorder: drug treatment
Bipolar disorder therapy is mainly based on mood-stabilizing drugs such as lithium, antiepileptic drugs and atypical neuroleptics. Since both the manic and the depressive phases must be treated, doctors often use different drugs.
If the mood-stabilizing active ingredients are not sufficient for the acute treatment, the doctor or therapist prescribes additional tranquilizers (sedatives) and antidepressants. Commonly used drugs are:
|
active substance |
application |
frequent side effects |
|
lithium (e.g., Quilonum) |
|
|
|
carbamazepine (e.g., Tegretal, Timonil) |
|
|
|
Valproic acid (e.g., Ergenyl, Orfiril) |
|
|
|
Tricyclic antidepressants (eg Saroten) |
|
|
|
Selective serotonin reuptake inhibitors (e.g., cipramil) |
|
|
The effect of these drugs often starts after a few weeks. Those affected must be patient at first, until the improvement is felt.
It is important to adhere to the exact prescriptions of the doctor when taking the medication. An independent increase in the dose is very dangerous and can cause serious side effects. Under no circumstances should the medication be stopped suddenly and without consultation with the doctor. This usually causes a renewed thrust of manic-depressive illness.
Bipolar Disorder: Wake Therapy
Even a so-called watch therapy can improve the depressive symptoms. The patient does without a night on his sleep. Surprisingly, this stabilizes the state of mind. If this method shows a good effect, sleep deprivation can be repeated.
This form of therapy must be carried out under medical supervision, as sleep deprivation can also trigger a manic phase. By combining with drugs, however, this risk can be reduced.
Bipolar disorder: electroconvulsive therapy
Electroconvulsive therapy works on both depressive and manic symptoms. In this therapy, the patient electrodes are created that produce a short-term seizure under general anesthesia. That sounds frightening, but it’s actually harmless.
For one thing, the patients in general anesthesia do not get any of it. On the other hand, this procedure has significantly fewer side effects than most medications. It is especially used when sufferers are severely affected by bipolar disorder or have a high risk of suicide.
While the effect of the medication only starts after a few weeks, the electroconvulsive therapy has an immediate effect. Before performing the procedure, the physician checks for existing risks, such as heart disease. Electroconvulsive therapy can not be used during pregnancy or in old age.
Bipolar Disorder: Psychotherapeutic Treatment
Interpersonal and Social Rhythm Therapy (IPSRT) and Family Focused Therapy (FFT) have proven to be particularly effective therapeutic treatments for bipolar disorder. Often, clinics also offer Cognitive Behavioral Therapy.
Cognitive behavioral therapy
In the IPSRT In addition to the reduction of personal difficulties, it is all about stabilizing the rhythm of life. Regular and adequate sleep reduces the risk of a manic or depressive phase. In the therapeutic sessions, the patients are informed about the bipolar disorder and learn how they can better structure their everyday lives.
The Family-focused therapy is preferred especially in younger patients. Important caregivers such as the parents or the partner are included in the therapy.
The advantage of this method is that even the caregivers are informed in detail about the bipolar disorder. In addition, opportunities are being worked out together on how normal everyday life can be carried out despite the illness. A communication and problem-solving training should reduce existing conflicts.
Behavior therapy helps the patient to recognize the early warning signs of bipolar disorder. Stress reduction is also an important part of the therapy, as stress plays a decisive role in the onset of pathological phases. The patient also learns to handle the medication carefully and learns strategies for dealing with manic and depressive symptoms.
Living with the disease
Bipolar disorder often accompanies patients for a lifetime. It is important for them to learn to deal with this condition in order to achieve a good quality of life. Psychotherapeutic treatment also helps those affected to integrate into their social and professional environment.
Bipolar disorder: disease course and prognosis
Is a bipolar disorder curable? This question is concerned as well as relatives. In fact, the mood swings disappear in a good third of the patients permanently. However, the greater part of those affected is accompanied by a bipolar disorder for a lifetime.
course
A bipolar disorder is very different individually. The course of the disease also depends on the type of bipolar disorder. In the classic form, the bipolar I disorder, manic and depressive phases alternate – sometimes in close intervals.
In bipolar II disorder, the depressive phases predominate and only so-called hypomanic phases occur. In cyclothymia, both the manic and the depressive phases are weak.
However, this does not mean that sufferers with a bipolar II disorder or cyclothymia have a lower level of suffering. Because in these forms of bipolar disorder, the manic or depressive episodes often occur more frequently than in the bipolar I disorder.
Mood swings in intervals
The depressive and manic phases usually last between eight and twelve weeks. Between these episodes, those affected can be symptom free for a long time. In the special form called “rapid cycling”, at least four stages of mania or depression occur over the year.
Early illness, unfavorable course
Bipolar disorder usually occurs for the first time between the ages of 15 and 25 years. The earlier the bipolar disorder occurs, the less favorable is usually the course.
According to studies, young patients are more suicidal and often have other mental disorders. Experts estimate the rate of suicide in bipolar patients at around 15 percent.
Early diagnosis important
It is important that a bipolar disorder is diagnosed as soon as possible. Left untreated, the manic and depressive phases occur more often. The more manic or depressive episodes a patient has gone through, the worse the treatment will usually be. Conversely, this means that a timely drug therapy can significantly improve the course.
Unfortunately, relapses can not be ruled out. The symptoms of bipolar disorder and thus the suffering can be significantly reduced by the medication.
Additional information
Books:
- The Bipolar Splits: Understanding Manic-depressive Humans (Donna Reynolds, TRIAS, 2011)
- Guide Bipolar Disorders: Help for Everyday Life (Daniel Illy, Urban & Fischer Verlag / Elsevier GmbH, 2016)
Guideline:
- S3 Guideline “Diagnosis and Treatment of Bipolar Disorders” of the German Society for Psychiatry and Psychotherapy, Psychosomatics and Neurology e.V.
Support group:
- DGBS – German Society for Bipolar Disorders e.V.