The bronchitis (acute bronchitis) is an inflammation of the mucous membrane in the bronchi. It is usually triggered by viruses and heals by itself within a few days. Bronchitis can also cause complications. Read now: What causes bronchitis? What to do about the complaints? What helps with bronchitis with complications? How long does a bronchitis take?

Acute bronchitis: short overview
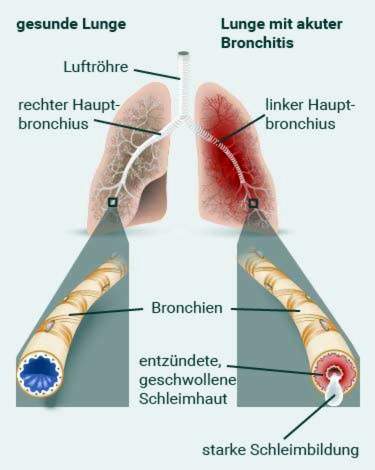
- What is bronchitis exactly? Inflammation of the mucous membrane in the bronchi (conducting “channels” from the trachea to the alveoli).
- symptoms: Cough (initially dry, later with sputum), possibly also fever, headache, throat and limb pain, runny nose, hoarseness
- Treatment: Protection, sufficient drinking, inhale, possibly cough remedy, with strong irritant cough (without expectoration) possibly cough suppressant (only in the evening); in certain cases antibiotics and / or cortisone
- Causes: in 90 percent of cases viruses, in almost 10 percent of cases bacteria; Rare bronchitis causes include fungi, inhaled irritants (such as ammonia, gastric acid) and radiation in cancer therapy
- complications: additional bacterial infection in viral bronchitis, pneumonia, spastic bronchitis
- Forecast: Acute bronchitis usually heals without any medical treatment. For complications and longer duration of bronchitis a visit to a doctor is advisable.
Acute bronchitis: symptoms and course
Acute bronchitis is usually triggered by cold viruses. That’s why she often occurs together with or after a cold on. One of the most important bronchitis symptoms is to cough: Most patients have one first dry irritated cough, He is often of sniff accompanied.
In about half of the cases, the viruses spread throughout the body. Then develops in bronchitis fever, Often, too cold symptoms such as sore throat, headache and body aches, hoarseness and a burning sensation behind the sternum. The affected people feel sick and unwell.
By the way: Bronchitis without cough is very rare. The fever may be missing. It only occurs when the whole body is affected by the virus infection.
In the further course of the disease, the symptoms change: Bronchitis patients develop after a few days a “productive coughIn the lower respiratory tract (bronchi), mucus dissolves, which is coughed off Cough with expectoration.
The coughed up mucus is usually viscous and clear to whitish, This is typical of the acute viral infection of the bronchial mucosa. In some patients, the discolored Expectoration yellowish or greenish. Then bacteria have settled on the inflamed mucous membranes. Doctors call this one bacterial superinfectionor bacterial secondary infection: A bacterial infection has “put on” the virus infection.
Bronchitis: signs of complications
In severe cases bronchitis patients cough Mucus with blood from. The blood usually comes from small injuries of the mucous membrane. This is not dangerous in general. But bloody expectoration can also have a serious cause. He should therefore always be medically clarified.
If the mucous membrane produces more mucus, swells and narrows, has one complicated bronchitis developed. It is also called obstructive or spastic bronchitis (see below). There are audible breath sounds (Rattling, wheezing). Some patients also get bad air (difficulty in breathing).
Sometimes, an acute bronchitis causes one lung infection (Pneumonia).
If bronchitis causes the following symptoms, you should definitely go to the doctor:
- The cough lasts longer than eight weeks.
- The patient has a very high fever, or the fever returns after a fever-free period.
- The patient feels very ill, has chills and night sweats.
- The coughed mucus contains blood.
- There is an increased amount of breathlessness. In addition, conspicuous, whistling breath sounds are audible.
People with weakened immune systems should go to the doctor even with mild bronchitis symptoms. The same applies to people with chronic heart or lung diseases (such as heart failure, COPD, asthma).
Bronchitis & pregnancy
Pregnant women should consult the doctor for bronchitis-like symptoms. It can rule out more serious causes of the symptoms (such as whooping cough). In addition, it makes sense to have the course of bronchitis during pregnancy monitored by a doctor – especially in case of complications. The doctor may also advise pregnant women on the selection of appropriate medication for the symptoms of bronchitis.
Bronchitis: treatment
“What to do with bronchitis?” With this question, especially in the cold season, many people turn to the doctor, pharmacist or to a health website on the Internet. The correct answer: There are no special bronchitis medications. Such would not be necessary in most cases. A simple bronchitis is uncomfortable, but not dangerous. Simple measures such as protection, sufficient drinking and inhaling are sufficient. This can alleviate the symptoms and support the healing process.
Dissolving phlegm is especially important
The fact that the lower respiratory tract increasingly produces mucus in bronchitis is an important defense mechanism: Together with the secretion, pathogens and dead cells are to be coughed off and thus removed from the body. To treat an acute bronchitis is called therefore above all drink enough.So the mucus dissolves better and can be easily coughed off. With it you support the infection defense.
Also Inhale helps to liquefy and dissolve the mucus. The same can be done if you use the chest carefully tap, Take the hollow hand or the little finger edge.
Many patients rely on expectorants (“HustenlöserThey contain N-acetylcysteine or ambroxol as the active ingredient, but so far it has not been scientifically proven that such preparations are actually helpful in acute bronchitis therapy.
Cough removers only work if you take a lot of fluids (tea, clear soup, etc.).
Do not suppress coughing!
In agonizing, unproductive coughing (without sputum) many patients can not sleep well. In addition, the constant, hard cough irritates the affected mucosa additionally. Many patients then take medicines that suppress the onset of cough (antitussives such as codeine). Colloquially, they become “cough suppressants“or”cough suppressantSome have a prescription and are more effective Other cough suppressants are over-the-counter (such as those with clobutinol), but their efficacy has been scientifically proven to be ambiguous.
If you want to use cough suppressants, you should only do so if heavy, dry cough attacks disturb your sleep. The purpose of coughing is to remove the germs from the airways. This defense mechanism should therefore only be suppressed for a short time, if you can not sleep otherwise.
In particular, prescription cough suppressants should apply only for a short time. They contain opiates like codeine. These harbor a certain addictive and addictive potential. In addition, they can make you very tired, reduce your ability to react and cause constipation.
If you have a productive cough (cough with sputum) you should not take any cough suppressants. The mucus in the bronchi must be coughed up. In addition, you must not combine cough suppressants with cough removers: The many liquefied mucus may otherwise accumulate in the bronchi.
Bronchitis: antibiotics only for bacterial infection
Many patients want to take antibiotics for bronchitis to recover quickly. But that rarely makes sense. Because bronchitis is a viral infection. In contrast, no antibiotics help. These are effective only against bacteria.
Therefore, the doctor prescribes an antibiotic for bronchitis only if on the attacked mucosa additionally bacteria have spread (bacterial superinfection). This can be seen, for example, from the fact that the coughing mucus is discolored by pus yellowish or greenish.
Cortisone in bronchitis
The effect of antibiotics in bronchitis with bacterial superinfection can be strengthened if you take additional short-term cortisone tablets. They have an anti-inflammatory effect. They are also useful in obstructive (spastic) bronchitis. Cortisone causes the mucous membrane in the airways to swell. The bronchial mucus, which contains plenty of germs and waste, can be better transported away. Inhaled cortisone is often recommended for obstructive (spastic) bronchitis.
More tips
If the bronchitis is accompanied by a cold or flu, fever, neck, head and body aches may occur. If necessary, you can do it Painkiller like ibuprofen or paracetamol. They lower the fever and relieve the pain. Ibuprofen also has anti-inflammatory effects.
Recommend medics physical conservation in bronchitis. Sport is therefore not useful during the acute illness, especially not with fever. Then you should get better bed rest comply.
The rooms where bronchitis patients are should be not overheated be. It is also important that the Air not too dry is. You can, for example, hang damp cloths over the heater or “breathe” regularly. A certain humidity does the mucous membranes well.
Bronchitis: home remedies
Many people use medicinal plants for bronchitis. For example, ribwort and Icelandic moss have a calming effect on the irritated mucous membrane. The medicinal plants are drunk, for example, as tea or used in the form of ointments, liquid extracts or lozenges. Even a full bath with suitable herbs can be very beneficial in acute respiratory diseases such as acute bronchitis.
A popular home remedy are also envelopes and chest wraps. They are made with quark, onions or boiled and mashed potatoes.
Read more about the best home remedies for bronchitis treatment in the article bronchitis – home remedies.
Acute bronchitis: causes and risk factors
The acute bronchitis will mostly by viruses triggered. Often these are cold viruses: The common cold is infection and inflammation of the upper respiratory tract. It can spread down into the bronchi. Then an acute bronchitis develops.
There are other viruses that can cause acute bronchitis. These include, for example, rhino, influenza, herpes, corona and parainfluenza viruses. Viral bronchitis in children is often caused by the RS virus (respiratory syncytial virus).
Rare is one Bronchitis by bacteria caused mainly by mycoplasma or chlamydia. Other bacteria are also possible. These include streptococci, staphylococci, pneumococci and Haemophilus influenzae. These are mainly responsible for acute bronchitis in immunocompromised people, lung patients and hospital patients.
More common than a purely bacterial bronchitis is a so-called bacterial superinfection in viral bronchitis: The attacked by the virus mucosa is then colonized by bacteria.
Very rare cause mushrooms an acute bronchitis. This happens especially in people whose immune system is weakened.
Other rare bronchitis causes are ammonia, hydrochloric acid, sulfur dioxide and nitrous gases. When inhaled, they damage the mucous membrane of the bronchi and can thus trigger inflammation. Irradiation (radiotherapy) in the context of cancer can be the reason for acute bronchitis.
For allergic persons, the contact with the allergy trigger can acute allergic bronchitis cause.
Bronchitis: incubation period
The period between infection with a pathogen (viruses, bacteria, fungi, etc.) and the appearance of the first symptoms is called the incubation period. Bronchitis caused by such germs can break out at different rates. Viruses are particularly fast: In a viral bronchitis, the incubation period is only one day. The additional colonization of bacteria on the mucous membranes in viral bronchitis can take up to ten days.
Is bronchitis contagious?
Acute bronchitis is contagious when it is caused by pathogens (viruses, bacteria, fungi). For example, when the patient coughs, he distributes tiny droplets of liquid with the germs in the ambient air. If a healthy person inhales this, he may also become ill.
However, not every infection leads to disease outbreaks: Bronchitis pathogens often only get ill if the infected person is weakened (for example, by a cold). Smog, smoking, cold and tobacco smoke are also considered risk factorsthat promote acute bronchitis.
Acute bronchitis: examinations and diagnosis
An acute bronchitis can usually be treated without medical help at home. You should at least have your family doctor examine you for severe bronchitis. He is good at assessing possible risks and dangers. Specialists in respiratory diseases are pulmonologists and ENT specialists. In acute bronchitis, however, they must be consulted only very rarely.
In any case, a doctor’s visit is advisable in the following cases:
- Difficulty breathing, shortness of breath and chest pain
- Cough of blood
- high fever
- yellowish or greenish expectoration
- Complaints lasting more than seven days
- Pre-existing conditions such as COPD, bronchial asthma or heart failure
- Immunodeficiency in HIV infection, cancer or cortisone therapy
- acute bronchitis in the elderly or children
Doctor-patient conversation and physical examination
The doctor will first ask you exactly about your symptoms – what symptoms they have, what color the phlegm has, how pronounced the symptoms are and since when they persist. Inform him also about possible pre or basic illnesses (cold, flu, asthma etc.). Through this conversation, the doctor can raise your medical history (anamnesis). It provides him with important information on the cause of her symptoms and on possible complications.
After that, the doctor will examine you. First of all, he will use the stethoscope heart and Listen to the lungs, In bronchitis in addition to the normal breathing sounds rattling, whistling or humming. These sounds are caused by the mucus that vibrates in the bronchi when the air passes by. In children, a so-called tube breathing notice.
The doctor will too Tap chestto judge the knocking sound. This provides indications of possible secretion congestion or effusions in the lungs. In addition, the doctor scans the lymph nodes on his neck and looks into the mouth, throat and ears. Often he also measures body temperature, heart rate and blood pressure.
A blood test is usually not necessary. It is carried out when the doctor suspects pneumonia: the direct connection of the bronchi and the lungs can cause pneumonia to develop from bronchitis.
In addition, a blood analysis can sometimes help to clarify the suspicion of a bacterial infection in bronchitis: If the erythrocyte sedimentation rate and the number of white blood cells are greatly increased, bacteria have probably settled on the mucous membranes of the respiratory tract. Then a treatment with antibiotics may be useful.
However, there are also bronchitis patients with bacterial infection, in which all blood levels are normal. Then the doctor can ejection or one Nasal or throat swab have them examined in the laboratory. Thus, the exact cause of bronchitis can be determined. If necessary, the doctor will then initiate a targeted antibiotic therapy.
A X-rays of the ribcage (Chest x-ray) is needed if you suspect pneumonia. In addition, it can exclude more serious causes of the symptoms, such as lung cancer in bloody sputum and worsening symptoms. In such a case, further examinations may be indicated, for example bronchoscopy.
When complicated bronchitis becomes a Lung function test (Spirometry) performed. So the doctor can determine if the airways are narrowed (such as spastic bronchitis).
Acute bronchitis: prognosis
The prognosis of acute bronchitis is very good. In most patients, it heals without any medical treatment without any problems. The duration of bronchitis varies: In uncomplicated cases, it usually resolves after a few days to a maximum of four weeks. A dry cough may persist for a longer period of time (up to eight weeks). But go to the doctor for a longer duration of illness. Bronchitis may not be aptly diagnosed, or chronic acute bronchitis has developed from the acute.
Bronchitis: complications
Caution is advised in elderly or immunocompromised patients as well as those with existing lung diseases. With them, the acute bronchitis can easily lead to complications, such as pneumonia. This is especially true if the bronchitis is abducted or not properly cured. As a result, the bronchitis can also become chronic.
In COPD patients, acute bronchitis can trigger a disease episode: COPD symptoms then deteriorate acutely.
Pneumonia and a bacterial superinfection are among the most common complications of acute bronchitis. Rarer develops a so-called “bronchiolitis obliterans”. In the process, the smallest bronchial branches (bronchioles) become inflamed and subsequently scarred. They then remain permanently closed, that is: This part of the airways narrows. Especially toddlers are prone to bronchiolitis obliterans.
Spastic bronchitis
Acute obstructive or spastic bronchitis is particularly prevalent in infants and toddlers. It is a complication of acute viral bronchitis. In spastic bronchitis the mucous membrane of the bronchi forms a lot of mucus and is at the same time swollen, so narrowed. This makes breathing difficult. The difficulty in breathing can even be threatening. In addition, when exhaling a Gills, whistles and / or drones audible.
The small patients receive special medication for respiratory distress, so-called sympathomimetics. These agents are often used as a spray or inhalation. They expand the airways. Then the patient’s breathing becomes easier again. In certain cases this will be special acute bronchitis also treated with other medications.
Read more about this special form of acute bronchitis in the article Spastic bronchitis.
Additional information:
guidelines:
- Guideline “Diagnosis and Therapy of Adult Patients with Acute and Chronic Cough” of the German Society for Pulmonology (as of 2015)