The tube stomach is a form of reduction of the stomach for the treatment of obesity. During the operation, a large part of the stomach is removed, so that only a hose-like remainder is maintained and the patients thereby feel much more satiated during eating. Read all important information about the requirements for the operation, its benefits and its risks!
What is a tube stomach?
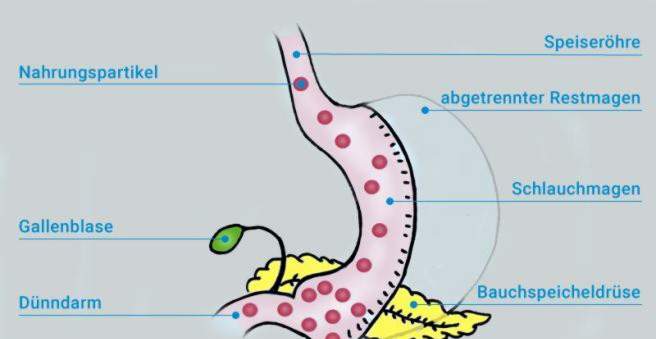
Tubular gland surgery or sleeve gastrectomy (sleeve) is a reduction surgery of the stomach for the treatment of obesity (adiposity). The method is based on the principle of food restriction: The surgery reduces the volume of the stomach to about the size of a small banana. As a result, the stomach is already filled after small amounts of food. The stomach filling leads to an expansion of the stomach wall, which in turn triggers the satiety.
In addition, hormonal processes that curb appetite appear to be triggered by the tube stomach surgery. There is evidence that after a gastrostomy gastrectomy, the stomach produces lower levels of the so-called starvation hormone “ghrelin”, thereby further reducing appetite. At the same time appetite-suppressing messenger substances are released. These include, for example, “GLP-1” and “peptide YY”.
The messenger substances also have a favorable effect on various metabolic processes (metabolism). Therefore, the stomach-shrinking operations are increasingly referred to as metabolic surgery. For example, in many patients an existing diabetes mellitus (type 2 diabetes mellitus) improves markedly after the operation.
The tube stomach surgery is carried out worldwide with a strong upward trend. In Germany, sleeve gastrectomy is the most commonly performed procedure of obesity surgery.
Preparation for the tube stomach surgery
Before the actual operation, certain preliminary examinations are necessary. This includes a reflection of the esophagus, stomach and duodenum (esophagogastroduodenoscopy) to exclude pathological changes such as inflammation, ulcers or tumors. Upper abdominal sonography can also be used to assess the liver, gallbladder and pancreas. For anesthesia preparation, an ECG is also written and, if necessary, a pulmonary function examination (“Lufu”) is carried out.
Especially with very pronounced obesity (BMI over 40 kg / m2) with fatty liver, a so-called protein-rich liquid phase is recommended to the patient before the operation of the gastric tube. It starts about 10 to 14 days before surgery depending on the hospital. During this time, patients should only take liquid, protein-rich foods. The aim of the liquid phase is a slight weight loss and reduction of fatty liver. Precise information on the course of this preoperative liquid phase is obtained directly from the treating hospital.
Drainage of the tube stomach OP
In a tube stomach, most of the stomach is removed. Remain a two to three centimeters narrow tube (sleeve stomach) with a capacity of about 80 to 120 milliliters.
The tube stomach surgery always takes place under general anesthesia. In general, however, no large abdominal incision is necessary, but the procedure is performed as a so-called minimally invasive surgery (keyhole technique) on some small cuts in the abdominal wall. The actual surgery takes just over an hour and is usually done in these steps:
- After inserting the surgical instruments and the camera, the abdominal cavity is filled with a gas (usually carbon dioxide) to provide better accessibility and a view of the abdominal organs.
- Now the surgeon drives with a so-called stapler (stapler) along the curved lower edge of the stomach (large curvature). The stacker has two functions: Firstly, this separates the lower part of the stomach. At the same time, staples are introduced along the cut, which connect the wound edges and close the remaining gastric tube. A time-consuming seam by hand is therefore not necessary.
- The separated stomach portion is pulled with a so-called Bergesack of plastic through one of the working channels from the abdomen. Subsequently, a stomach tube is used to introduce dye into the stomach. This serves to check the tightness of the staple seam along the cutting edge. If no dye is released, the operation can be completed.
For whom a stomach is suitable
A tubular stomach is a great way to effectively reduce weight for overweight people from a body mass index (BMI) of 40 kg / m². For additional illnesses such as diabetes, which could improve by the weight loss, a tube stomach is also laid from a BMI of 35 kg / m².
The prerequisite is that the patient has already undergone several unsuccessful weight loss attempts (with a change in diet and lifestyle) under medical supervision. Patients should be at least 18 and 65 years old or less.
Hose stomach as an intermediate goal
In extremely overweight people, the tube stomach surgery is sometimes performed as a first step in a more complex obesity surgery. If the patient then lost weight and thereby reduced its surgical risk, in a second step, even more effective surgery is performed, such as a biliopancreatic division or gastric bypass. Such operations not only restrict food intake (restriction), but also food utilization (malabsorption).
For whom a stomach is not suitable
A tube stomach is unsuitable for people whose obesity is the result of eating soft, high-calorie foods or liquids, for example, many sweets, sweet-eater or alcoholic beverages. Because such Kalorienträger pass the tube stomach almost directly (they run through), without filling it and trigger a feeling of satiety
In these cases, a malabsorptive procedure such as gastric bypass is the more sensible option. Also unsuitable is the tube stomach for people with a reflux disease. Acid reflux and heartburn may continue to increase after surgery.
Efficacy of the peritoneal surgery
The chances of losing weight are very high in tubule surgery: Initial studies show that patients on average manage to reduce their excessive body weight between 33 and 83 percent. Since tubal gland surgery is a relatively recent surgical technique, there are no long-term results on the success of the method.
In some people, it comes after a few years of weight loss to a new weight gain. A certain orientation with regard to long-term expectations is provided by a technique very similar to the tube stomach, the so-called “Magenstraße-Mill-Operation”. In this operation, which is no longer usual, a gastric tube was also formed, but the remaining gastric portions were left in the body. This technique, which is comparable to the tube stomach, showed in a study a five-year result of 60 percent excess weight loss (EWL).
Advantages of a tube stomach over other methods
In contrast to other surgical procedures, the function of the stomach remains basically intact in a tubular stomach. The closure of the stomach entrance and exit is preserved. Therefore, patients can eat almost normal again after a postoperative, gradual diet – only smaller amounts.
The procedure is shorter and gentler than, for example, a gastric bypass surgery. On the other hand, sleeve gastrectomy is significantly more effective than gastric banding.
side effects
After surgery, patients need to have vitamin B for life12 artificially via injections (intramuscular or as a short infusion). Because the vitamin can not be absorbed by the intestine in sufficient quantities. The reason: Since a large part of the stomach is removed, this no longer forms enough “intrinsic factor” – a protein that is responsible for the absorption of vitamin B12 is required from the intestine.
Breast gland surgery can not be reversed if, for example, the patient has successfully reduced his weight.
Risks and complications
As with any surgery, problems or complications may occur during or following a gastric tube surgery. In addition to the typical risks of general anesthesia include:
- Injuries to blood vessels with bleeding or bleeding
- Injuries to other organs
- Disorders of wound healing or wound infections
- Leakage of the gastric suture (suture insufficiency) with transfer of gastric contents into the abdomen and the risk of peritonitis (Peritonitis)
- (transient) disorders of the gastrointestinal activity
- Adhesions of the abdominal organs
Sleeve gastrectomy has a lower complication rate compared to other obesity procedures. The individual risk depends to a large extent on the health of the patients.
Diet after surgery
After a tube stomach surgery, the diet is usually for about one to two weeks initially only from pass or liquid diet. The hospital then recommends a nutrition plan for the gradual diet. In the long term, the daily food intake is distributed to about five to seven smaller meals per day.
Basically, a few weeks after the tube stomach surgery again all food is allowed, provided that they are well tolerated. However, diet and lifestyle habits need to be fundamentally and permanently changed for effective weight loss. Of the Sleeve Gastrectomy is only one – albeit effective – building block in the context of obesity therapy.