Chlamydia infection is caused by bacteria. It can cause different clinical pictures. Depending on the Chlamydia subgroup, genital organs, eyes or respiratory tracts are particularly affected. Read all important information about: What are Chlamydia? What symptoms do they cause? How can you treat a chlamydia infection?

Chlamydia infection: short overview
- symptoms: Pharyngitis, (conjunctivitis (in case of infection of the eye), burning on urination, purulent discharge from urethra and testicular pain (men), pelvic pain, vaginal discharge and bleeding (women), itching on the anus, small skin ulcers, lymphadenopathy
- Infection: Droplet infection and saliva (C. pneumoniae), infectious tear fluid, unprotected intercourse (C. trachomatis), over birds (C. psittaci, notifiable!)
- Incubation period (from infection to onset of first symptoms): one to four weeks
- diagnosis: physical examination, smear, urine test, blood test for pathogens or antibodies, ultrasound (in case of suspected infection in the lower abdomen)
- Treatment: with the antibiotics azithromycin or doxycycline, ceftriaxone and metronidazole
- Watch out: For urogenital infections, the sexual partner must always be co-treated
- complications: Blindness (with eye infection), infertility (genitourinary infections), joint inflammation (Reiter’s disease), heart inflammation
Chlamydia: symptoms
Chlamydia are bacteria that can cause a variety of conditions with different symptoms. The most well-known and by far the most common Chlamydia infection affects the urinary and genital organs (urogenital chlamydia infection). This sexually transmitted venereal disease Chlamydia can affect both women and men alike.
In addition, certain chlamydia infects the eyes, lungs and other organs in severe cases.
In total, there are three types of Chlamydia that can cause diseases in humans:
- Chlamydia trachomatis
- Chlamydia (Chlamydophila) psittaci
- Chlamydia (Chlamdyophila) pneumoniae
Chlamydia symptoms due to Chlamydia trachomatis
There are several subgroups (serovars) of the bacterium Chlamydia trachomatis that cause various diseases:
- trachoma: Chlamydia signs on the eye; caused by the serovars A to C
- Infections of the urinary and genital organs (urogenital infections), Conjunctivitis: caused by serovars D to K
- Lymphogranuloma venereum: a venereal disease; caused by the serovars L1 to L3
In addition to special symptoms, in principle, any infection can also flu symptoms such as fever, headache and body aches. In addition, some patients with chlamydia complain of fatigue and weakness throughout the day.
trachoma
The first infection with Chlamydia trachomatis serovar A-C usually occurs in childhood. It causes an acute first Conjunctivitis (Conjunctivitis). On the conjunctiva certain white blood cells accumulate in the form of tiny grains (follicles).
In poor hygienic conditions, the patients get infected again and again with Chlamydia (reinfection). In addition, other bacteria can “sit on” the inflammation (superinfection). Both factors cause the follicles to enlarge and aggregate into so-called granulomas.
The chronic inflammation shrinks the inner mucous membrane of the eyelids scarred. As a result, the eyelid edges arch with their eyelashes inside and irritate the cornea of the eye (trichiasis) by small injuries. This inflames itself (keratitis) and becomes increasingly cloudy. In the end, the person concerned go blind.
Urogenital chlamydia symptoms in men
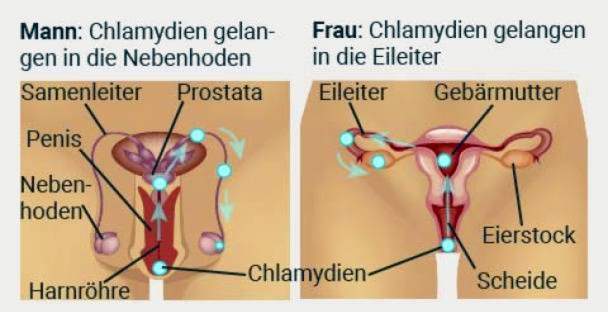
Serovars D to K trigger urogenital infections. The signs of chlamydia-infected urinary and genital organs in men usually affect the urethra: it inflames (urethritis). The patient feels a pressure sensation and painful burning while urinating, The Chlamydia may cause it discharge of pus from the urethra.
The germs can rise up in the prostate as well as in the testicles and epididymis: It develops a prostate inflammation (Prostatitis), testicle inflammation (Orchitis) or epididymitis (epididymitis). Pain and infertility (Sterility) are the possible consequences.
Many infected men also show no symptoms due to chlamydia, Physicians then speak of an asymptomatic infection.
Urogenital chlamydia symptoms in the woman
In women, Chlamydia trachomatis D-K infection can cause cervicitis and / or urethritis. A possible indication of chlamydia in cervicitis is slimy-purulent, often strong-smelling discharge, Urethritis can be frequent urination and pain or Problems with urination be accompanied.
However, most women even have chlamydia-related cervicitis and / or urethritis no complaints, The infection then usually goes unnoticed and is not treated. This can have dire consequences:
The bacteria can continue to rise: The inflammation then spreads to the uterine lining, fallopian tubes and ovaries. In summary, medics speak of one here inflammatory pelvic disease (pelvic inflammatory disease, PID). Again, many sufferers do not have chlamydia symptoms. Others complain, for example Lower abdominal pain, atypical discharge, bleeding in the middle of the cycle or after intercourse.
In severe cases, serious late effects threaten. This includes chronic pelvic pain and infertility, In addition, there is an increased risk of the fertilized egg implanting outside of the uterus during pregnancy (extrauterine pregnancy, for example) ectopic pregnancy).
In some women, the inflammatory pelvic disease attacks the peritoneum (peritonitis). The liver capsule can also inflame (perihepatitis = Fitz-Hugh-Curtis syndrome). Possible chlamydia symptoms in this case are in addition fever and fatigue right hand Epigastric pain and a tender painful liver, The pain can radiate up to the right shoulder. The inflammation can also spread to the adjacent tissue of the cecum (periappendicitis).
Chlamydia symptoms in men and women
Especially through anal and oral sex chlamydia in men and women can also reach the rectum and throat. There, inflammation can develop. Of the inflammation of the fundus (proctitis), many sufferers notice nothing, because no complaints occur. Other infected people complain of chlamydia symptoms like Itching on the anus and bloody-purulent Stuhlbeimengungen.
Chlamydia-related pharyngitis can be associated with a reddened throat, sore throat and sore throat express. In addition, the germs can also affect the eye and trigger conjunctivitis there.
Chlamydia symptoms in pregnant women and newborns
Infection with Chlamydia trachomatis during pregnancy can have the same consequences as with non-pregnant women. Cervix and / or uterine lining may be ignited. This can have serious consequences like premature birth or premature rupture of membranes, Also the risk for others pregnancy complications can increase.
In addition, the bacteria can be transmitted to the baby at birth. The risk is 50 to 70 percent. typical Chlamydia symptom in the newborn is then usually a conjunctivitis, more rarely a middle ear infection. If the child inhales germ-containing vaginal fluid during birth, severe pneumonia is threatened.
In the postpartum period, some infected mothers develop inflammation of the endometrium (postpartum endometritis).
Lymphogranuloma venereum
This sexually transmitted disease is caused by Chlamydia trachomatis serovars L1 to L3. She starts with painless little blistersfollowed by superficial skin ulcers at the infected parts of the body. These are usually in the genital area. After about ten to thirty days the surrounding people swell lymph node (Groin) painful. Often the skin is discolored blue-red.
In some cases, the lymph nodes break up, and pus leave. When healing, connective tissue forms scar, In addition, lymphatic vessels can be relocated. The lymph can then no longer drain properly and builds up. The genitals can thereby enlarge extremely (elephantiasis).
Common chlamydia symptoms in this disease are fever, headache, muscle and joint pain.
Through anal intercourse the infection can also affect the rectum. The lower intestinal sections become inflamed (proctosigmoiditis). The sufferers have slimy-bloody outflows, Spasms in defecation (Tenesmen) and fever, Even abscesses and fistulas in the rectum area can form. When healed, scarred constrictions may occur in the rectum.
Chlamydia Symptoms by Chlamydia psittaci
Chlamydia (Chlamydophila) psittaci causes a condition called ornithosis (or psittacosis). She can act as gripal infect or atypical lung infection express. Atypical pneumonia is when it is not caused by the most common pathogen (streptococcus).
Key symptoms of Chlamydia psittaci infection include body aches, chills and fever around 39 degrees Celsius. In addition, dry, irritant coughing initially occurs. Later, the cough is accompanied by little expectoration.
In severe cases, this chlamydial infection can spread to other organs, such as the heart muscle. Then one can Myocarditis Develop (myocarditis).
Some people who become infected with Chlamydia psittaci develop no symptoms at all.
Chlamydia symptoms due to Chlamydia pneumoniae
The pathogen Chlamydia (Chlamydophila) pneumoniae affects the respiratory tract and causes inflammation. For example, one can Inflammation of the paranasal sinuses (Sinusitis), one sore throat (Pharyngitis) or one bronchitis develop. The chlamydia infection can also be atypical lung infection to lead. Depending on the location of the inflammation, sufferers complain of throat, swallowing and chest pain, for example. Headache, fever and cough are also possible chlamydia signs in this infection.
Chlamydia: causes and risk factors
Chlamydia are immobile bacteria, which occur in two forms: Outside of the cells of an infected, they are present as so-called elementary bodies. In this form they are contagious (infectious).
But to multiply, chlamydia must first enter a host cell. That can be about a human mucosal cell. Inside the cell, the bacteria are present as reticulum bodies: they are no longer infective, but metabolism and are capable of dividing. They undergo a development cycle in the host cell that spans several days. In the end, they transform into elementary bodies. These are released from the host cell – either by being expelled or after the host cell has been destroyed. The new elementary particles can now infect neighboring cells or be transferred to other individuals.

Chlamydia transmission
How this infection with Chlamydia occurs depends on the type of pathogen:
Chlamydia: transmission of Chlamydia trachomatis
In Chlamydia trachomatis, the serovars D to K and L1 to L3 are mainly by intercourse transfer. The infection takes place via the colonized mucous membranes of the urethra, vagina, penis and rectum. Also body fluids such as vaginal secretions, urine and semen (also the “pleasure drops”) can pass on pathogens. In addition, a pregnant woman infected with these serovars can transfer the bacteria to the newborn at birth.
Chlamydia transmission with serovars A through C is by infectious eye fluid, Even contaminated hands or textile products (such as towels or washcloths) can infect themselves with these chlamydia. A Chlamydia transmission by flies was also observed in this subgroup. Therefore, the pathogen is widespread, especially in countries with poor hygienic conditions.
Chlamydia: transmission of Chlamydia pneumoniae
This bacterium will over the air and over salivary fluid transfer. It collects and multiplies like Chlamydia trachomatis in human cells. Also in some animals (like koala bears or horses) one finds such Chlamydien. Contagion routes to humans are not known.
Chlamydia: transmission of Chlamydia psittaci
Chlamydia psittaci disease is called ornithosis (bird disease). The reason is that chlamydia transmission through infected birds takes place. These are the natural host of the bacteria. The most important sources of infection for humans are turkeys, ducks, parrots and pigeons. Like humans, they may develop Chlamydia psittaci or be completely symptom-free. Especially in ornamental birds, the bacterium can accumulate for a long time without causing disease.
Chlamydia transmission to humans takes place via the faeces and the feathers of infected animals. Even the mere touch can already lead to Chlamydia infection. In liquid discharges from the beak or respiratory tract of the birds are also chlamydia.
Human-to-human routes of infection are unknown in Chlamydia psittaci.
Chlamydia: incubation period
Chlamydia affects the mucous membranes of the genital and anal regions as well as the respiratory tract. However, until the first signs of disease develop, many diseases pass some time. This time between contagion and outbreak is called incubation time. It is one to three weeks in Chlamydia trachomatis. Psittaci and pneumoniae strains take about one to four weeks.
Regardless, the duration of infectiousness of Chlamydia. However, since many infections remain asymptomatic, they can hardly be determined.
Risk factors for a Chlamydia infection
Different chlamydia types are transmitted in different ways. Therefore, different risk factors of infection apply:
Chlamydia trachomatis: risk factors
For sexually transmitted chlamydia (Chlamydia trachomatis D-K and L1-L3), the following risk factors apply in particular:
- Oral Sex
- Vaginal traffic, especially unprotected (= without a condom)
- Anal intercourse, especially unprotected
- sharing contaminated and unprotected sex toys
Who already has the HI virus (HIV) is at an increased risk of contracting chlamydia. The AIDS pathogen weakens the human immune system so that it can fight chlamydia and other pathogens worse.
Conversely, in the case of Chlamydia infection, the risk of becoming infected with HIV: The inflamed mucosal cells in the genital area represent an ideal portal of entry for the HI virus.
The serovars D-K of Chlamydia trachomatis can also trigger conjunctivitis. “swimming pool conjunctivitis“Is the colloquial name of this disease due to chlamydia. Oral Here, however, is a much larger risk factor than swimming in a swimming pool: The germs, for example, about the sperm fluid in the eye.
A risk factor for conjunctivitis due to Chlamydia trachomatis A-C (trachoma) is mainly poor hygiene at a low standard of living. The infection is therefore particularly in underdeveloped countries.
Chlamydia pneumoniae: risk factors
Bacteria of this genus are distributed worldwide. In Germany, too, a high degree of contamination of the population is assumed. So, probably every person has at least once in his life contact to Chlamydia pneumoniae. There are no specific risk factors for chlamydia transmission here. As with most infectious diseases, the risk of infection increases due to a weak immune system, increasing age and direct contact with infected people.
Chlamydia psittaci: risk factors
Chlamydia psittaci is particularly susceptible to bird breeders, traders and ornamental birds. Even dried bird excrement and feathers can be contagious for up to four weeks. If the infected birds are not treated, about ten percent of them develop into chronic, but asymptomatic germ carriers.
Chlamydia infection: diagnosis and examination
If you suspect that your urinary or genital organs are infected with chlamydia, you should consult a doctor Urologists, Women to gynecologists (Gynecologist) go. Also a dermatologist is a specialist for skin and venereal diseases a suitable contact person.
In a Chlamydia-related respiratory disease (such as pneumonia), should the family doctor be the first port of call. Chlamydia infection on the eye can give you a ophthalmologist help.
Medical history (anamnesis)
The doctor will first talk to you about yours medical history rise. For example, he asks about typical symptoms and possible pre-existing conditions. Suspected Chlamydia infection in the genital area also information on sexual habits are significant. Possible questions are:
- Have you noticed unusual discharge from your urethra / vagina? If so, what does it look like?
- Do you feel pain or a burning sensation while urinating?
- Do you suffer from itching in the genital area, especially at the anus?
- Do you change your sexual partner more often?
- Have you recently had unprotected intercourse?
- Do you have other pain, for example in the abdominal and pelvic region?
- Have you noticed any swelling in the area of the testis or groin?
If you also have throat and sore throat, oral chlamydia transmission may be the cause. Answer your doctor openly for appropriate inquiries. Only then can he determine the exact cause of your complaints.
Trachoma occurs mainly in tropical countries. Therefore, if you have any eye pain or redness, you will be asked about previous trips.
For respiratory ailments, the doctor will ask for the exact symptoms and any contacts with birds:
- Do you have a cough? Is this dry or with ejection?
- Do you suffer from chills or fever?
- Do you feel knocked off?
- Do you work with birds or do you keep some?
Physical examination
After the detailed questioning follows the physical examination. For complaints in the urogenital area, the doctor will examine the genitals and the anus. In women, the gynecologist will examine the vagina and the cervix. In addition, the doctor scans surrounding lymph nodes.
He will also tap the belly, feel and listen. Inflammation of the internal female reproductive organs can sometimes be felt by the doctor as swelling under the abdominal wall. If he presses on the right upper abdomen, stabbing pains point to a chlamydia infection of the liver capsule.
To diagnose a chlamydia infection of the respiratory tract, the doctor must tap the lungs (percussion) and listen with a stethoscope (auscultation). In throat and swallowing complaints, a reddened throat may indicate mucosal inflammation (pharyngitis).
If a Chlamydia infection of the eye is suspected, the doctor examines this in detail for redness or inward-rotated eyelids (entropion).

Imaging procedures
Imaging examinations such as computed tomography (CT) or ultrasound (ultrasonography) are usually not necessary for chlamydia infection.
However, Chlamydia trachomatis bacteria can penetrate up to the abdomen, especially in women. Abscesses or other swelling due to inflammation of the fallopian tubes and ovaries (pelvic inflammatory disease) can be detected by the doctor in the ultrasound image. A chlamydia infection of the peritoneum and the liver capsule (perihepatitis) can cause free fluid in the abdomen. This can be seen on CT scans.
Chlamydia test
There are different types of Chlamydia testsDirect methods are intended to detect the pathogen itself in patient specimens. Indirect methods are searching for antibodies to chlamydia in the blood.
Chlamydia Test: Direct detection of bacteria
A chlamydia test for direct bacterial detection is used to test the suspicion of infection and to ensure the diagnosis. There are very different test procedures that differ in terms of their informative value and possible applications.
For example, the doctor may detect chlamydia in a swab taken from the cervical mucosa, urethra or rectum, for example. There is also a Chlamydia urine test, Particularly suitable is this chlamydia test in men for the detection of urogenital infection. Eye infections (secreted fluid) are investigated for eye infections.
In respiratory infections, tissue (biopsy) and mucus from infected lung sections are used as laboratory samples. These can be obtained by lung reflections (bronchoscopy). The sputum or pharynx can also be used for chlamydia tests.
To detect the Chlamydia in the sample material, the pathogens can be grown in a cell culture. This is partly difficult and for safety reasons only possible in specialized laboratories.
Alternatively, one can detect certain structural components of the bacteria, such as characteristic proteins on the surface of the germs. Some are based on such antigen tests Chlamydia rapid test.
Another option is to detect the Chlamydia genome in the sample material. This is usually done by so-called nucleic acid amplification tests (NAAT). They are now considered the method of choice.
Chlamydia test: Detection of antibodies
Upon infection with chlamydia, the immune system reacts with the formation of specific antibodies. It may take a few weeks for these to be detected in the patient’s blood. Therefore, such a serological chlamydia test is generally not suitable for detecting an acute infection.
However, if the germs ascend in a genitourinary Chlamydia infection and infect pelvic or abdominal organs, they are often no longer detectable in smears such as from the cervix or from the urethra. In such cases, Chlamydia antibodies can often be found in the blood.
A serological chlamydia test makes sense to clarify an ascended (complicated) chlamydia infection. Also, to determine the cause of infertility, the doctor can take a blood sample and have them tested for Chlamydia antibodies. Because an infection can cause sterility as a late consequence.
Chlamydia test costs and Chlamydia screening
Women up to the age of 25 can get one free once a year Chlamydia screening test at the gynecologist. For this chlamydia screening, a patient’s urine sample for Chlamydia trachomatis is examined. The costs are borne by the statutory health insurance companies.
Women who want to be tested after the age of 25 as a precautionary measure for chlamydia must bear the costs themselves. The same goes for men of all ages. An exception is a doctor-prescribed chlamydia test: men and women are then examined and tested for free.
Chlamydia: test also for sexual partners
If you have been diagnosed with Chlamydia trachomatis, your sexual partners should also be examined and treated at least for the last six months. Because even if they have no complaints, they may be infected with chlamydia. If only you are treated alone, you can get infected again after the treatment has finished with your sexual partner.
Chlamydia infection: treatment
A chlamydia infection is having antibiotics treated. Most often, in the doxycycline used. This representative of tetracyclines blocks chlamydia growth. Other antibiotics used in chlamydia treatment include azithromycin, erythromycin and ofloxacin.
The selection of chlamydia antibiotics and their dosage depend inter alia on the clinical picture (trachoma, urogenital infection, etc.). Women also consider whether they are pregnant or breastfeeding. In addition, the doctor pays attention in the treatment planning to possible additional infections. On the inflamed by chlamydia mucous membranes may in addition spread other pathogens.
Treatment of Chlamydia trachomatis infections
The chlamydia treatment in this type of pathogen depends primarily on the clinical picture.
Those who are infected with chlamydia but show no symptoms generally receive doxycycline. The infected person must take 100 milligrams of the antibiotic twice a day for seven days. Alternatively, a single dose of 1.5 grams of azithromycin may be prescribed. This may be useful for patients who would not take doxycycline reliably for a week.
Chlamydia treatment for urogenital inflammation
An acute one urethritis Chlamydia is also preferably treated with doxycycline in men and non-pregnant women (100 milligrams daily for seven days). Also an acute one prostatitis and cervicitis Chlamydia are usually treated with this regimen.
In men, this chlamydia treatment can be extended to 14 days if the Inflammation on the seminal vesicles or epididymides has overreached.
If inflammation has spread to the fallopian tubes and / or ovaries in women, there is a “pelvic inflammatory disease“(PID). Here, the doctor will prescribe a combined chlamydia therapy of several antibiotics (ceftriaxone, doxycycline, metronidazole). The duration of treatment is one to two weeks, depending on the course of the disease.
For all genitourinary Chlamydia infections also the Sexualpartner mitbehandelt become. This prevents couples from repeatedly infecting each other with chlamydia.
Chlamydia treatment in Lymphogranuloma venereum
The Chlamydia STD is also mostly treated with doxycycline. Patients must take 100 milligrams of the antibiotic twice a day for 21 days.
The alternative is chlamydia therapy with azithromycin (once) or erythromycin (over 14 days). However, these antibiotics are considered second choice drugs.
Chlamydia treatment during pregnancy and lactation
If pregnant or nursing women suffer from genital chlamydia infection, the doctor prefers azithromycin: The patient must take a single dose of the antibiotic.
Alternatively, the doctor may prescribe chlamydia therapy with erythromycin. This antibiotic must be taken for one to two weeks depending on the dose.
Of the sexual partners The patient must also be examined and treated for Chlamydia.
Chlamydia treatment in newborns
Babies who contract Chlamydia trachomatis with their infected mother during labor are usually treated with erythromycin. The antibiotic is given over 14 days.
Alternatively, chlamydia treatment in neonates can also be done with azithromycin. Sometimes a single dose is enough. In other cases, the antibiotic is given for three days.
Chlamydia treatment for rectal or pharyngitis
The chlamydia therapy of choice in one Rectal inflammation (Proctitis) or sore throat (Pharyngitis) is doxycycline: For seven days, take 100 milligrams of the antibiotic twice a day. Alternatively, the antibiotic azithromycin may be given.
When the patients at the same time to the venereal disease Gonorrhea (gonorrhea) The doctor chooses a combination therapy: He prescribed the two antibiotics ceftriaxone and azithromycin.
Chlamydia treatment for eye infections
Chronic connective and corneal inflammation is caused by the serovars A to C of Chlamydia trachomatis trachoma called. The chlamydia therapy usually consists of the one-time intake of 1.5 grams of azithromycin. Alternatively, the antibiotic may also be applied locally (for example as an ointment) over several days.
A Conjunctivitis by the Chlamydia serovars D to K can also be treated with a single dose of 1.5 grams of azithromycin. But there are also other options for chlamydia therapy: For example, the doctor may prescribe a lower dose of azithromycin or doxycycline. The intake must then take place over several days. Alternatively, as with trachoma, topical azithromycin administration may be used.
Chlamydia treatment in other pathogens
Chlamydia treatment for Chlamydia psittaci or Chlamydia pneumoniae infection generally consists of doxycycline: patients must take the antibiotic for ten to 21 days.
Alternatively, other antibiotics can be prescribed. These include, for example, erythromycin or azithromycin.
By the way: Acute infections with Chlamydia psittaci are notifiable.
Chlamydia Treatment: More Tips
Je nach Krankheitsbild kann man die antibiotische Chlamydien-Behandlung mit weiteren Maßnahmen unterstützen.
Beispielsweise empfehlen Mediziner bei einer urogenitalen Chlamydien-Infektion und Lymphogranuloma venereum, während der Behandlung auf Geschlechtsverkehr zu verzichten.
Besonders bei schweren urogenitalen Infektionen kann der Arzt für einige Zeit Schonung und Bettruhe empfehlen – zusätzlich zur Therapie mit Antibiotika.
Chlamydien-Beschwerden einer Nebenhoden- oder Hodenentzündung lassen sich oft lindern, indem die Hoden hochgelagert werden. Dafür eignet sich ein „Hodenbänkchen“, etwa aus einem zusammengerollten Handtuch. Zusätzlich sollte man die Hoden kühlen, etwa mit feucht-kalten Umschlägen.
Bei einer Chlamydien-bedingten Harnröhrenentzündung sollte man viel trinken, Empfehlenswert sind vor allem mild desinfizierende Nierentees, beispielsweise aus Hauhechelwurzel, Bärentraube oder Birkenblättern.
Fragen Sie am besten Ihren Arzt, wie Sie selbst die medikamentöse Chlamydien-Behandlung wirksam unterstützen können!
Chlamydien-Infektion: Krankheitsverlauf und Prognose
Bei rechtzeitiger und konsequenter Behandlung heilen Chlamydien im Allgemeinen folgenlos aus. Viele Chlamydien-Infektionen bleiben aber zunächst unerkannt, da sie kaum Beschwerden verursachen. Das gilt besonders auch für eine Chlamydien-Geschlechtskrankheit: Infizierte sind dadurch eine unbewusste Ansteckungsquelle für Sexualpartner.
Chlamydien: Komplikationen
Unbehandelt kann eine Chlamydien-Infektion chronisch werden und Komplikationen verursachen:
Unfruchtbarkeit und Extrauterine Schwangerschaft
Eine urogenitale Infektion kann im Körper aufsteigen: Bei Männern kann es so zum Beispiel zu einer Hoden- und Nebenhodenentzündung kommen. Die Patienten können unfruchtbar werden.
Bei Frauen kann eine urogenitale Chlamydien-Infektion ins kleine Becken aufsteigen und dort zu Entzündungen etwa der Eileiter und Eierstöcke führen. In der Folge können diese verkleben und vernarben. Das erhöht das Risiko für Unfruchtbarkeit und für Schwangerschaften außerhalb der Gebärmutter (Extrauteringravidität) wie Eileiter- oder Bauchhöhlenschwangerschaft.
Zudem kann die Entzündung auf das Bauchfell und die Leberkapsel übergreifen (Perihepatitis = Fitz-Hugh-Curtis-Syndrom). Auch hier kann es zu Verklebungen kommen.
Reaktive Arthritis (Reiter-Syndrom)
Eine Entzündung der Harnröhre durch Chlamydia trachomatis kann in seltenen Fällen eine reaktive Arthritis nach sich ziehen. Diese Form von Gelenkentzündung wird auch Morbus Reiter oder Reiter-Syndrom genannt. Sie tritt vor allem bei Männern auf.
Die meisten Patienten weisen drei Symptome auf (Reiter-Trias genannt): eine nicht-eitrige Harnleiterentzündung, eine schmerzhafte Gelenkentzündung (Knie-, Sprunggelenk etc.) und eine Bindehautentzündung.
Weitere mögliche Anzeichen von Morbus Reiter sind Hautausschläge etwa im Bereich der Genitalien, der Mundschleimhaut und der Fußsohlen. Ebenfalls möglich sind Komplikationen wie Entzündungen des Herzmuskels (Myokarditis), des Rippenfells (Pleuritis) und der Hauptschlagader (Aortitis).
Weitere Komplikationen bei Chlamydien
Eine Infektion mit Chlamydia psittaci kann beispielsweise eine Entzündung des Herzmuskels, des Herzbeutels und der Herzinnenhaut (Myo-, Peri- und Endokarditis) verursachen. Manche Patienten entwickeln auch eine Entzündung oberflächlicher Venen mit einer Blutgerinnsel-Bildung (Thrombophlebitis). Auch das Zentrale Nervensystem kann an den Entzündungsprozessen infolge einer Chlamydia psittaci-Infektion beteiligt sein.
Sehr selten führt auch eine Infektion mit Chlamydia pneumoniae zu Entzündungen im Bereich des Herzens (Myokarditis und Endokarditis). Ebenfalls nur vereinzelt beobachtet man Komplikationen wie schmerzhaft knotige Hautrötungen (Erythema nodosum), Morbus Reiter oder Entzündungen der Rückenmarksnerven oder Hirnhäute (Meningoradikulitis).
Chlamydien-Infektion bei Neugeborenen
Rund 50 bis 70 Prozent der infizierten Schwangeren übertragen bei der vaginalen Geburt die Chlamydien auf das Kind. Als Folge entwickelt das Neugeborene meist eine Bindehautentzündung und/oder eine Lungenentzündung. Letztere wird in vielen Fällen von einer Mittelohrentzündung begleitet.
Chlamydien vorbeugen
Um einer sexuell übertragbaren Chlamydien-Infektion vorzubeugen, sollten Sie stets ein Kondom beim Geschlechtsverkehr benutzen. Das gilt sowohl für den Vaginal- als auch den Analverkehr. Auch beim Oralverkehr sollte man zum Schutz vor einer Ansteckung ein Kondom beziehungsweise ein „Lecktuch“ (Dental Dam“) verwenden.
Eine Bindehautentzündung durch Chlamydia trachomatis (Trachom) ist die weltweit häufigste Augenkrankheit und die zweithäufigste Ursache für eine Erblindung. Sie ist vor allem in Ländern mit schlechten Hygienestandards verbreitet. Wer in solchen Ländern unterwegs ist, sollte deshalb besonders auf Hygiene achten.
Bei Chlamydia pneumoniae gibt es keine speziellen Vorbeugemaßnahme. Risikopersonen wie chronisch kranke, ältere oder immungeschwächte Menschen sollten den Kontakt mit Erkrankten meiden.
Um sich nicht mit Ornithose anzustecken, sollten Sie den Kontakt mit Vögeln meiden, die mit Chlamydia psittaci infiziert sind. Schutz vor einer Ansteckung bieten auch Schutzkleidung, Mund- und Nasenschutz. Denn bereits durch den Kontakt mit verunreinigtem, kontaminiertem Staub können die Chlamydien übertragen werden.
Weiterführende Informationen
Leitlinien:
- S2k_Leitline “Infektion mit Chlamydia Trachomatis” der Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften e.V.(Stand: 2016) http://www.awmf.org/leitlinien/detail/ll/059-005.html
- S1-Leitlinie “STI/STD Beratung, Diagnostik und Therapie” der Deutschen STI-Geselschaft (DSTIG) et al. (Stand:2015) http://www.awmf.org/leitlinien/detail/ll/059-006.html